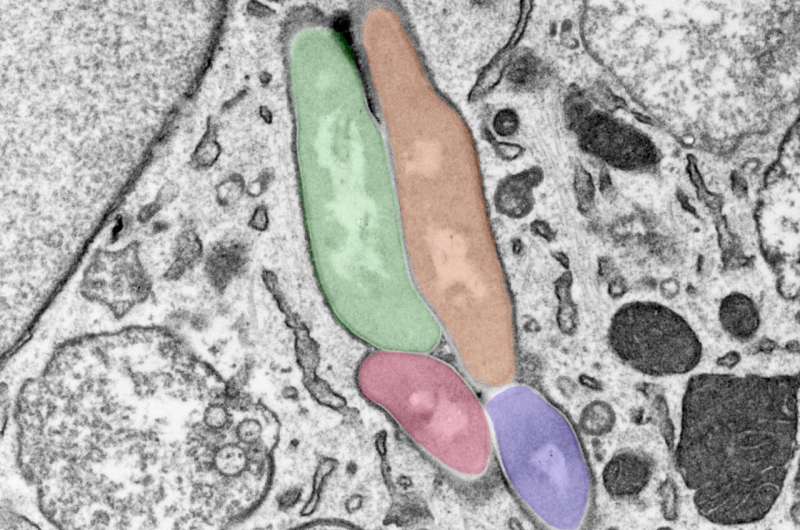
Image showing a macrophage infected with several M. tuberculosis bacilli (pseudocolored in different colors). Credit: Tony Fearns (Host Pathogen Interactions in Tuberculosis Lab)
Researchers at the Francis Crick Institute have found that the body's process of removing old and damaged cell parts is also an essential part of tackling infections that take hold within our cells, like TB.
If this natural process can be harnessed with new treatments, it could present an alternative to, or improve the use of antibiotics, especially where bacteria have become resistant to existing drugs.
In their study, published in Nature Microbiology today, ahead of World TB Day on the March 24, the team studied genes that are key to bacteria's ability to evade autophagy, a pathway that cells use to destroy themselves when they are under stress or infected.
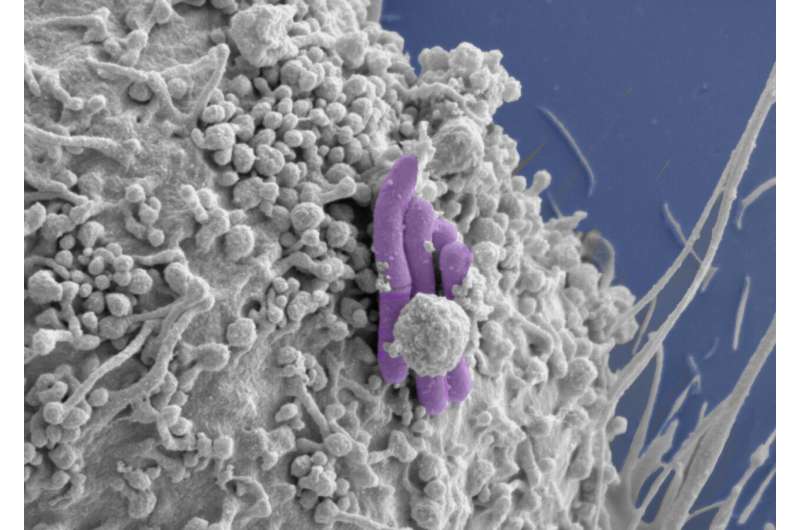
They engineered human immune cells called macrophages from specialist stem cells called induced pluripotent stem cells, which have the ability to become any cell type in the body. They then used genome editing tools to manipulate the macrophages' ability to perform autophagy. When genes important to autophagy were removed and the cells were infected with Mycobacterium tuberculosis (bacilli that cause TB), the bacterial infection took hold, replicating more within the engineered cells and causing mass host cell death.
These results are evidence for the strong role of autophagy in controlling intracellular infections like TB. If this pathway can be boosted or strengthened, it could be a new avenue for tackling antibiotic resistance, by making existing antibiotic drugs more effective or presenting an alternative to drugs in cases where bacteria have evolved resistance.
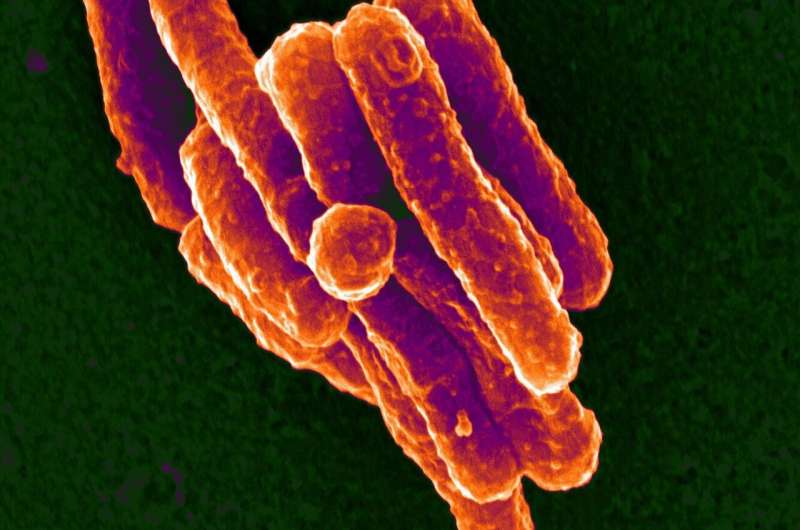
Mycobacterium tuberculosis, the bacteria that causes human tuberculosis. Credit: Max Gutierrez (Host Pathogen Interactions in Tuberculosis Lab)
Max Gutierrez, head of the Host-Pathogen Interactions in Tuberculosis Laboratory at the Crick, said, "I first studied the role of autophagy in infection during my Ph.D., so it's incredible to see renewed interest in this field. Using the latest technologies, we've been able to show a key role for this pathway in controlling infection.
"As immunotherapies have harnessed the immune system to fight cancer, boosting this immune defense with a host-directed therapy, could be a valuable new tool in the fight against infections, particularly those becoming resistant to antibiotics."
The team also validated their results using macrophages isolated from blood samples, confirming the importance of autophagy in human defenses.
Image of a macrophage (gray) infected with M. tuberculosis (pseudocolored purple), the bacilli bacteria that cause TB. Credit: Tony Fearns (Host Pathogen Interactions in Tuberculosis Lab)
Beren Aylan, joint first author and Ph.D. student at the Crick together with Elliott Bernard and Enrica Pellegrino, said, "Antibiotic resistance is a huge threat to our health so it's incredibly important to understand how our bodies fight infection and where there might be room for improvement.
"TB is a great example of where targeting our own immune defenses could be really effective, because it takes a very long course of different antibiotic treatments to effectively remove the infection. Anything that can be done to more effectively remove bacteria, could also make a huge difference to the cost and accessibility of treatments."
The team are now planning to screen for drug compounds that could be used to boost autophagy in a targeted way.
"Boosting the autophagy pathway isn't as simple as it might seem," adds Max. "This is because all parts of the body use autophagy as a way to recycle old and damaged cells. In order to safely increase autophagy in the location of infections, we need to target the pathway in macrophages alone."
More information: Harnessing power of immune system may lessen reliance on antibiotics for infections like TB, Nature Microbiology (2023). DOI: 10.1038/s41564-023-01335-9
Journal information: Nature Microbiology
Provided by The Francis Crick Institute