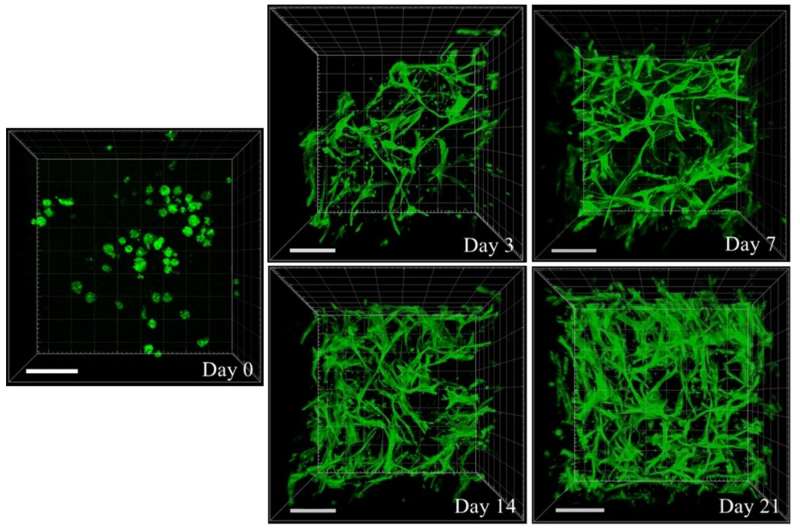
Figure shows the cell-conducive environment of gellan gum-collagen IPN hydrogels. The encapsulated adipose-derived mesenchymal stem cells (ADSCs) exhibit gradual return of morphology to their usual spindle-like shape over 21 days of culture. This shows that the cell-conducive environment of the IPN hydrogels facilitated cell adhesion, spread, and proliferation. F-actin (cytoskeleton) of cells were stained green with Phalloidin-iFluor 488 reagent and z-stack images were captured with confocal laser scanning microscopy (CLSM) using Zeiss LSM 710 to analyse the entirety of the cell-laden hydrogels at referred time points. Cell adhesion to, and cell spread within, IPN hydrogels could be observed in all 3 dimensions. (Scale bar: 100 µm) Credit: ACS Applied Bio Materials
NUS researchers have discovered a method to fabricate a biologic interpenetrating network (IPN) hydrogel using applied rheology.
Hydrogels are three-dimensional networks of crosslinked polymers. However, current hydrogel wound dressings are made up of synthetic polymers that are biologically inert and do not drive hosts' biology toward wound healing. Such treatment modality is particularly paradoxical for severe wounds where exogeneous mediators are critical for regeneration. Recently, the incorporation of stem cells has been proposed to confer inert dressings with biologic properties. The cells possess the ability to release paracrine wound-healing factors and differentiate into multiple skin cell types to replace lost tissues. In order to replicate aspects of the stem cells' native extracellular matrix (ECM) environment, researchers are turning to natural polymers that are more cytocompatible.
Sourcing from nature's repository, gellan gum, which is an exopolysaccharide secreted by the bacterium Sphingomonas elodea, is gaining recognition for its FDA GRAS and high-yield production status. Although it forms hydrogels readily under physiological conditions, gellan gum lacks cell adhesion moiety to effectively house stem cells. This can be overcome by incorporating a secondary collagen polymer network to confer gellan gum hydrogels with cell adhesivity.
However, gellan gum and collagen have opposing temperature-dependent gelation mechanisms. Using applied rheology, a research team led by Prof Rachel EE from the Department of Pharmacy, National University of Singapore developed a method to precisely control the temperature for an IPN hydrogel between gellan gum and collagen to form naturally. Her team's approach to transform gellan gum into a biologic scaffold with collagen is a significant improvement that may potentially lead to commercial development. Encapsulated stem cells using the IPN hydrogel were able to adhere to and proliferate within the gel matrix (see Figure). Further animal model experiments proved that the cell-laden IPN hydrogels were able to promote wound healing in severe burn injuries. This work is protected and patent is pending.
Prof Ee said, "Together with our partners in Roquette, we are committed to mine the rich diversity of plant-based materials for biomedical uses. Our work is an exciting example of how academia and industry can pool our resources for impactful discoveries."
More information: Jian Yao Ng et al. Pristine Gellan Gum–Collagen Interpenetrating Network Hydrogels as Mechanically Enhanced Anti-inflammatory Biologic Wound Dressings for Burn Wound Therapy, ACS Applied Bio Materials (2021). DOI: 10.1021/acsabm.0c01363
Provided by National University of Singapore