'Decoy' nanoparticles can block HIV and prevent infection
Flipping the standard viral drug targeting approach on its head, engineers at the University of California San Diego have developed a promising new "nanosponge" method for preventing HIV from proliferating in the body: coating polymer nanoparticles with the membranes of T helper cells and turning them into decoys to intercept viral particles and block them from binding and infiltrating the body's actual immune cells.
This technique, developed in the Nanomaterials and Nanomedicine Lab led by nanoengineering professor Liangfang Zhang, could be applied to many different kinds of viruses, opening the door for promising new therapies against difficult-to-combat viruses. Zhang is a professor in the Department of NanoEngineering at the UC San Diego Jacobs School of Engineering.
This HIV work first appeared in the journal Advanced Materials in November 2018 in a paper titled "T-Cell-Mimicking Nanoparticles Can Neutralize HIV Infectivity." The work is ongoing.
"The key innovation here is that we're standing on the other side of the big problem with HIV," said Weiwei Gao, a chemical engineer and associate project scientist in the Zhang Lab at the UC San Diego Jacobs School of Engineering. "The traditional drug development approach requires that we figure out how to block critical protein or signaling pathways in the virus so that it can't attack the body. The problem is that there are so many pathways and so much redundancy in these viruses, it's really difficult to find one pathway that's truly critical.
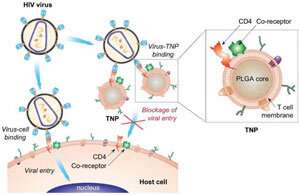
"Our approach comes from the other side: look at the virus target," he continued. "The nanoparticles are wrapped with the membranes of cells that the virus targets. Therefore, they can act as a decoy of the cell to intercept the viral attack."
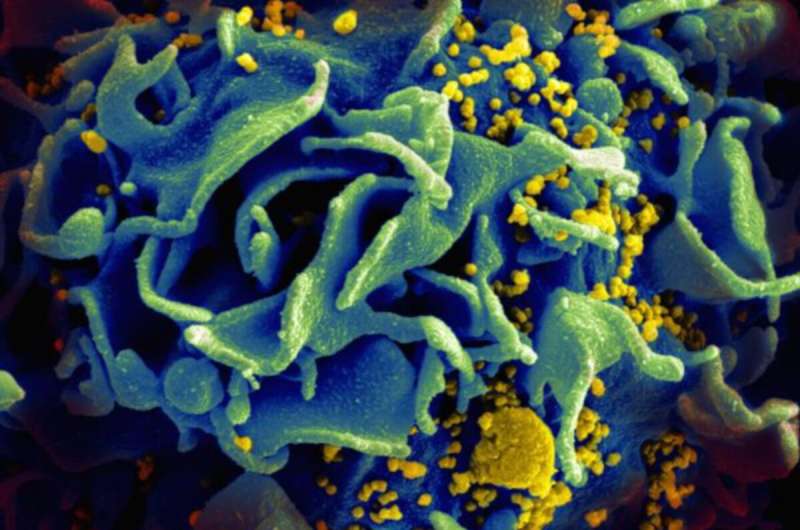
The HIV virus typically targets cells called CD4+ T cells; also called T helper cells, in the healthy body, these cells help detect foreign pathogens and target them for attack and removal. The HIV virus finds and binds to the surface of these T cells using the CD4 receptor, then injects their genetic material into the T cells and uses the T cell machinery to replicate itself. Eventually, after enough new HIV virus has been made, the viral particles burst out of the cell and search for other T cells to attack.
Part of why HIV is so devastating is that attacking and killing T cells severely damages the immune system, making it harder for the body to fight off secondary infections. And the virus mutates quickly, changing its genetic code and making it difficult to target with traditional antiviral and drug discovery methods.
In the 2018 Advanced Materials study, the researchers coated nanoparticles with the isolated cell membranes of CD4+ T cells. When added to T cells in a dish and exposed to viruses, these nanoparticles, called TNPs, acted like a sort of sponge, soaking up the virus and protecting the T cells from being infected. They found that the HIV virus was just as likely to bind to a TNP as it is to bind to a T cell—but since there's no cellular machinery inside these nanoparticles, the virus can't inject or replicate itself, and it is rendered harmless.
Just like with CD4+ T cells, the nanoparticles bind with HIV virus through the gp120 protein on the surface of the virus. When TNPs were added to the T cell mixture at a concentration of 3 mg/mL, the team saw a reduction of infection of over 80 percent, when compared to cells that had not been treated with TNPs. They take this as promising evidence that these nanoparticles could be infused into the bloodstream in patients to soak up the HIV infection, knocking down their infection levels and ultimately clearing it out of the system.
"There is another potential application of using TNPs to treat HIV. Immune cells in the body that are infected with HIV but are not actively producing new virus become viral reservoirs," said Gao. "Finding ways to destroy such reservoirs is a major challenge facing HIV researchers. But these reservoir cells may also express gp120, so TNPs can be used as vehicles to precisely deliver antivirals to these cells and kill them."
The work was inspired by earlier projects in Zhang's lab focused on red blood cells. "Our work has been focused on using nanoparticles for drug delivery," Gao said, "but nanoparticles don't circulate for long in the body. We had the idea: to make it harder for the body to recognize the nanoparticles as foreign, what if we disguise them as red blood cells? Red blood cells are naturally long circulating, so if we can mimic them with nanoparticles, we should see a similar circulation pattern." The team's work on the red blood cell cloaking technology first appeared in the academic literature in 2011 in the PNAS paper "Erythrocyte membrane-camouflaged polymeric nanoparticles as a biomimetic delivery platform."
Gao says this approach can likely be applied to a wide variety of pathogens. "Lots of bacteria also like to attack red blood cells," he said. "So maybe these nanoparticles can act as a decoy to block the toxins from the bacteria. Or they could act as decoys to react to other toxins, like nerve agents, that target red blood cells."
There are a number of obstacles still in their path before these TNPs can be used in human patients. For example, they have not yet been able to test their TNPs in living animal models.
"Because HIV is a human disease, it's difficult to replicate it in animal models," Gao said. "So we're working closely with Dr. Stephen Spector, the Chief of the Division of Pediatric Infectious Diseases at UC San Diego Health, on that issue, to figure out the best approach for testing this in vivo.
"Our study is really proof of concept," Gao continued. "The disease development changes at different stages of the disease, and the virus works differently inside the body, with different levels of infectivity and activity. It will be critical to work with doctors and researchers who are very familiar with HIV pathology to optimize the treatment regime based on what's known about the disease to be sure that the nanoparticles are the most effective for treatment."
Still, this work represents the first step in an exciting new direction for HIV treatment, and Gao sees the field as full of possibilities. "This technology is very adaptable, both for existing pathogens and for new, emerging diseases," he said. "This platform can overcome drug resistance, and can be easily adapted to use other cell membranes or load other drugs or treatments into the nanoparticle core. It's very modular, and doesn't require custom designs for each compound, which may help treatment development in the future."
More information: Xiaoli Wei et al. T-Cell-Mimicking Nanoparticles Can Neutralize HIV Infectivity, Advanced Materials (2018). DOI: 10.1002/adma.201802233
C.M. J. Hu et al. Erythrocyte membrane-camouflaged polymeric nanoparticles as a biomimetic delivery platform, Proceedings of the National Academy of Sciences (2011). DOI: 10.1073/pnas.1106634108
Journal information: Advanced Materials , Proceedings of the National Academy of Sciences
Provided by University of California - San Diego



















