Adhesive force differences enable separation of stem cells to advance therapies
A new separation process that depends on an easily-distinguished physical difference in adhesive forces among cells could help expand production of stem cells generated through cell reprogramming. By facilitating new research, the separation process could also lead to improvements in the reprogramming technique itself and help scientists model certain disease processes.
The reprogramming technique allows a small percentage of cells – often taken from the skin or blood – to become human induced pluripotent stem cells (hiPSCs) capable of producing a wide range of other cell types. Using cells taken from a patient's own body, the reprogramming technique might one day enable regenerative therapies that could, for example, provide new heart cells for treating cardiovascular disorders or new neurons for treating Alzheimer's disease or Parkinson's disease.
But the cell reprogramming technique is inefficient, generating mixtures in which the cells of interest make up just a small percentage of the total volume. Separating out the pluripotent stem cells is now time-consuming and requires a level of skill that could limit use of the technique – and hold back the potential therapies.
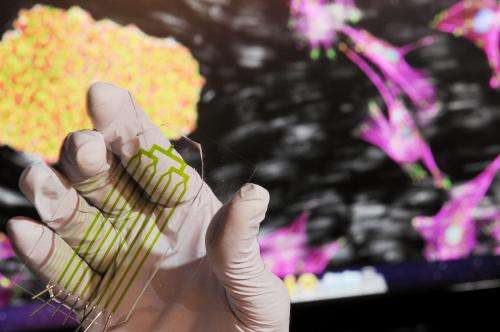
To address the problem, researchers at the Georgia Institute of Technology have demonstrated a tunable process that separates cells according to the degree to which they adhere to a substrate inside a tiny microfluidic device. The adhesion properties of the hiPSCs differ significantly from those of the cells with which they are mixed, allowing the potentially-therapeutic cells to be separated to as much as 99 percent purity.
The high-throughput separation process, which takes less than 10 minutes to perform, does not rely on labeling technologies such as antibodies. Because it allows separation of intact cell colonies, it avoids damaging the cells, allowing a cell survival rate greater than 80 percent. The resulting cells retain normal transcriptional profiles, differentiation potential and karyotype.
"The principle of the separation is based on the physical phenomenon of adhesion strength, which is controlled by the underlying biology," said Andrés García, the study's principal investigator and a professor in Georgia Tech's Woodruff School of Mechanical Engineering and the Petit Institute for Bioengineering and Bioscience. "This is a very powerful platform technology because it is easy to implement and easy to scale up."
The separation process will be described April 7 in the advance online publication of the journal Nature Methods. The research was supported by the National Institutes of Health (NIH) and the National Science Foundation (NSF), supplemented by funds from the American Recovery and Reinvestment Act (ARRA).
"The scientists applied their new understanding of the adhesive properties of human pluripotent stem cells to develop a quick, efficient method for isolating these medically important cells," said Paula Flicker, of the National Institutes of Health's National Institute of General Medical Sciences, which partly funded the research. "Their work represents an innovative conversion of basic biological findings into a strategy with therapeutic potential."
An improved separation technique is essential for converting the human induced pluripotent stem cells produced by reprogramming into viable therapies, said Todd McDevitt, an associate professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University, and director of Georgia Tech's Stem Cell Engineering Center.
"For research purposes, depending on labeling reagents for separation is not a major problem," said McDevitt, one of the paper's co-authors. "But when we move into commercialization and manufacturing of cell therapies for humans, we need a technology approach that is unbiased and able to be scaled up."
The separation technique, called micro stem cell high-efficiency adhesion-based recovery (µSHEAR), will allow standardization across laboratories, providing consistent results that don't depend on the skill level of the users. "Because of the engineering and technology involved, and the characterization work, we now have a technology that is readily transferrable," McDevitt said.
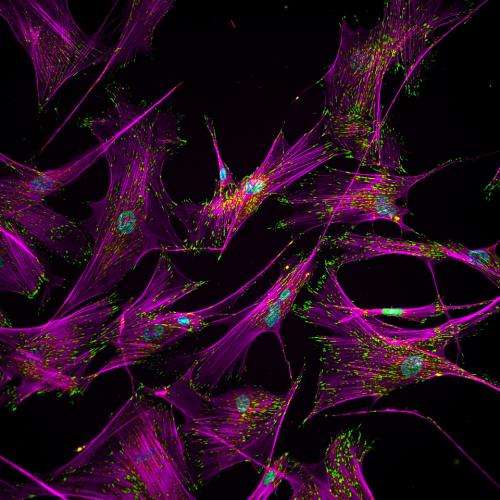
The µSHEAR process grew out of an understanding of how cells involved in the reprogramming process change morphologically as the process proceeds. Using a spinning disk device, the researchers tested the adhesive properties of the hiPSCs, the parental somatic cells, partially-reprogrammed cells and reprogrammed cells that had begun differentiating. For each cell type, they measured its "adhesive signature" – the level of force required to detach the cells from a substrate that had been coated with specific proteins.
The research team, which included Georgia Tech postdoctoral fellows Ankur Singh and Shalu Suri, tested their technique in microfluidic devices developed in collaboration with Hang Lu, a professor in Georgia Tech's School of Chemical and Biomolecular Engineering.
In the testing, cells from the culture were first allowed to attach to the substrate before being subjected to the flow of buffer fluid. Cells with a lower adhesive signature detached from the substrate at lower flow rates. By varying the flow rate, the researchers were able to separate specific types of cells, allowing production of stem cell cultures with purity as high as 99 percent – from mixtures in which those cells accounted for only a few percent of the total.
"At different stages of reprogramming, we see differences in the molecular composition and distribution of the cellular structures that control adhesion force," García explained. "Once we know the range of adhesive forces for each cell type, we can apply those narrow ranges to select the populations that come off in each range."
Using inexpensive disposable "cassettes," the microfluidic system could be scaled up to increase the volume of cells produced and to provide specific separations, García noted.
Unlike existing labeling techniques, the new separation process works on cell colonies, avoiding the need to risk damaging cells by breaking up colonies for separation. The separation process has been tested with both reprogrammed blood and skin cells. Cells were provided for testing by ArunA Biomedical, a company based in Athens, Ga., founded by University of Georgia professor Steven Stice.
Beyond the direct application in producing stem cells, the separation technique could also help scientists with other research in which cells need to be separated – including potential improvements in the reprogramming technique, which won the Nobel Prize for medicine in 2012.
"Cell reprogramming has been a black box," said McDevitt. "You start the reprogramming process, and when the cells are fully reprogrammed, you can pick them out visually. But there are really interesting scientific questions about this process, and by isolating cells undergoing reprogramming, we may be able to make new discoveries about how the process occurs."
Journal information: Nature Methods
Provided by Georgia Institute of Technology















