Antibiotics are unique assassins
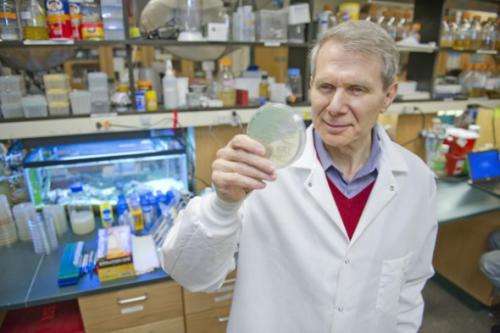
In recent years, a body of publications in the microbiology field has challenged all previous knowledge of how antibiotics kill bacteria. "A slew of papers came out studying this phenomenon, suggesting that there is a general mechanism of killing by antibiotics," said Kim Lewis, University Distinguished Professor in the Department of Biology and director of Northeastern's Antimicrobial Discovery Center.
The standard thinking at the time was that the three main classes of bactericidal antibiotics each had a unique way of killing bacterial cells—like specialized assassins each trained in a single type of weaponry. But this new research suggested that all antibiotics work the same way, by urging bacterial cells to make compounds called reactive oxygen species, or ROS, which bacteria are naturally susceptible to.
"If they were right it would have been an important finding that could have changed the way we treat patients," said Iris Keren, a senior scientist in Lewis' lab.
And that's exactly how science usually works, said Lewis—through challenges to mainstream thinking. But recent results reported by Lewis, Keren, and their research partners in an article published Friday in the journal Science suggest that this alternative hypothesis doesn't hold up. For example, even bacteria that are incapable of making ROS are still vulnerable to antibiotics. Further, some antibiotics can work their fatal magic in both aerobic and anaerobic conditions—but reactive oxygen species can only form when there's oxygen to fuel them.
"We chose to do the simplest and most critical experiment aimed at falsifying this hypothesis," said Lewis. "Killing by antibiotics is unrelated to ROS production," the authors wrote. The findings were corroborated by University of Illinois researchers in another study released on Friday .
The team treated bacterial cultures with antibiotics in both the presence and absence of oxygen. Other than the gaseous environment, the two treatments were identical. There was no difference in cell death between the two populations.
Before performing these experiments, Lewis' team first looked at signals of a fluorescent dye, which previous researchers had used as an indicator for ROS levels. The team treated bacterial cells with a variety of antibiotics and measured the strength of this signal. Since antibiotics were presumed to increase ROS levels, one would have expected increased concentrations of antibiotics to correlate with stronger signals. However, Lewis' group saw no such correlation.
"But there's a difference between correlation and direct observation," Keren said. In order to support their observations with unequivocal data, the team members physically separated the cells that had stronger fluorescent signals from those with weak signals and treated them both with the same antibiotics. Both populations suffered equivalent cell death.
"The research from Dr. Lewis' group demonstrates that, contrary to current dogma, antibiotics apparently do not kill bacteria through induction of reactive oxygen species," said Steven Projan, vice president for research and development at iMed and head of Infectious Diseases and Vaccines at MedImmune, both subsidiaries of AstraZeneca. "The results shown are rather clear but still leave us with the mystery as to how antibacterial drugs help infected people clear bacterial infections. At this point, we should probably dispense with the 'one size fits all' approach to bacterial killing by antibiotics," said Projan, who was not involved in the research.
With these results, Lewis and Keren hope the field will be able to focus its efforts on understanding the true mechanisms of how antibiotics wipe out bacteria in order to effectively address chronic bacterial infections, one of the most pressing issues facing public health today.
Journal information: Science
Provided by Northeastern University


















