This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Scientists identify potential new method for diagnosing male infertility
Researchers have discovered a new phenomenon where sperm from mice can induce non-reproductive cells from hamsters to fuse and form a syncytia—a cell with multiple nuclei.
The study, published today in eLife, finds that the degree of this multinucleation is dependent on the fertilizing potential of the sperm. With further validation, the findings could be used in the development of new diagnostic tools for male infertility.
According to the World Health Organization, infertility is estimated to affect about 15% of the world's population. Possible solutions include assisted reproductive techniques, such as in vitro fertilization (IVF). Previously, the hamster oocyte penetration test was used as a way to quantify the ability of a sperm to fertilize an egg—its fusogenic potential. However, this test is now considered obsolete, so there is no current standardized way to specifically analyze the fusogenic potential of a patient's sperm.
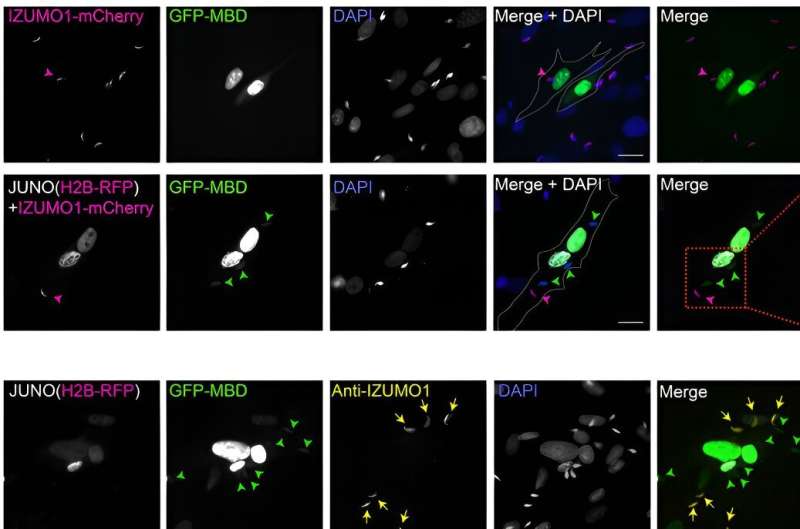
"In mammals, the fusion of the sperm to the plasma membrane of the egg is mediated by the interaction between two proteins: IZUMO1 on the sperm, and JUNO on the egg, or oocyte," explains co-author Clari Valansi, a Lab Manager at the Department of Biology, Technion—Israel Institute of Technology, Haifa, Israel.
"In our previous work, we showed that mouse sperm can fuse to a type of connective cell called fibroblasts that have been altered to express JUNO," adds co-author Nicolas Brukman, a postdoctoral researcher at the Department of Biology, Technion—Israel Institute of Technology. "In this study, we looked to further investigate the mechanisms of mammalian sperm-oocyte fusion."
The team started by incubating sperm from adult mice with Baby Hamster Kidney (BHK) cells that had been genetically modified to express JUNO. The team was surprised to discover that the sperm cells induced the BHK cells to fuse together and form one cell with multiple nuclei, or a syncytia. This effect was also observed when using the Human Embryonic Kidney cells.
They determined that this multinucleation was dependent on the presence of JUNO. However, this alone was not sufficient to induce the process. Rather, only cells with sperm fused to them formed syncytia, and the level of multinucleation was found to be dependent on the amount of sperm added to the cells. This suggests that the fusion of sperm with JUNO-expressing BHK cells is needed to induce the subsequent multinucleation of the BHK cells.
Next, the team asked whether the multinucleation required JUNO to be present on both fusing BHK cells. They employed a content-mixing experiment in which two populations of cells expressing different fluorescent markers were mixed and exposed to the mouse sperm. There was no BHK-BHK fusion when only one or neither of the cell populations expressed JUNO, suggesting that the sperm-induced multinucleation was indeed dependent on all of the BHK cells expressing JUNO. The team has dubbed this process SPICER (SPerm-Induced CEll-cell fusion Requiring JUNO).
Finally, the team evaluated the potential of SPICER in determining the fusogenic potential of sperm. They incubated mouse sperm in media that prevent capacitation—the process by which sperm acquires its fusogenic capacity—and found that they were subsequently unable to fuse to BHK cells and induce syncytia formation. Furthermore, fully capacitated sperm incubated with an antibody that blocks IZUMO1 also failed to form multinucleated cells.
To examine whether the extent of cell-cell fusion relates to the sperm's fertilizing capability, the team assessed the levels of multinucleation in parallel with the performance of the sperm during IVF. They detected a significant positive correlation between syncytia formation and the levels of fertilization. Taken together, these results suggest that SPICER relies on fully capacitated sperm, as well as the sperm's fertilizing potential, supporting its potential use as a diagnostic tool for male infertility.
The authors call for more research in this area to validate their findings. Future experiments using human sperm would be required to fully realize the potential of SPICER in diagnostic settings.
"We have described a new phenomenon in which sperm cells can induce the fusion of cells expressing JUNO in culture, resembling the viral-like fusion of cells upon infection," concludes co-author Benjamin Podbilewicz, Professor of Biology in the Department of Biology, Technion—Israel Institute of Technology.
"As the extent of multinucleation was correlated with the sperm's fertilizing potential, SPICER could be a step towards the development of a reliable, fast, and simple method for predicting sperm function during the diagnosis of male infertility. It could also be used to predict the success of assisted reproductive techniques such as IVF, or in the agricultural world to evaluate the fertility of stud animals."
Nicolas Brukman, Clari Valansi, and Benjamin Podbilewicz are inventors on a patent application filed by the Technion-Israel Institute of Technology, based on this work.
More information: Nicolas G Brukman et al, Sperm induction of somatic cell-cell fusion as a novel functional test, eLife (2024). DOI: 10.7554/eLife.94228
Journal information: eLife
Provided by eLife




















