Quasi-distributed temperature sensors from draw-tower fabrication technology
Maturing draw-tower fabrication technology for optical fibre gratings has been used to produce quasi-distributed temperature sensors that could extend the use of RFTA in cancer treatment.
Taking temperatures
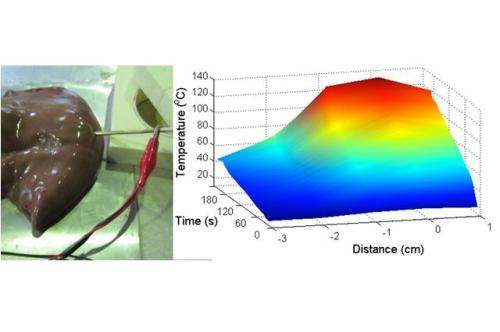
Radio-frequency thermal ablation (RFTA) is a technology used to heat and destroy tissue, to treat a range of medical problems. It is used in cardiac medicine to destroy heart tissue causing irregular heatbeats and it is used to remove several types of cancer by destroying tumour cells in the lungs, kidneys and liver. In RFTA, the required heat is generated by a mid-power RF field, terminated on a needle-like ablation device.
It is important to be able to monitor the temperature of the tissues around the RFTA device, especially in cancer treatment, where thermal dosimetry – the temperature reached and its persistence – is related to the rate of death of the tumour cells. Thermocouples and thermistors are used for temperature sensing in clinical RFTA, with the sensors inserted through the skin separately or, in some cases, embedded in the ablation device. These sensors need to be shielded to be compatible with MRI, which may be used to guide the procedures.
These kinds of sensor have several limitations, including response time, single point measurements and location. Thermocouples have response times of 1–10 seconds, giving discrete snapshots of the temperature over time. They can only provide the temperature at a single point, as it is not possible to have several thermocouples on a single cable. As for location, the thermocouple is often mounted within the hollow RFTA needle, leading to the sensor being heated more than the tissue.
The inherent MRI compatibility and small size of optical fibre devices makes them of interest for many applications in medicine, including RFTA temperature sensing. Optical fibre sensors based on fibre Bragg gratings (FBGs) do not need to be shielded from MRI, allow multiple sensing points in-line along a single thin fibre, have instantaneous response time and are small enough not to interfere with the RF irradiance.
Strength in distribution
In this issue of Electronics Letters, a team including members from the University of Limerick in Ireland and Italy's Politecnico di Milano report a quasi-distributed sensor incorporated in an RFTA device, using an emerging type of FBG; draw-tower gratings (DTGs).
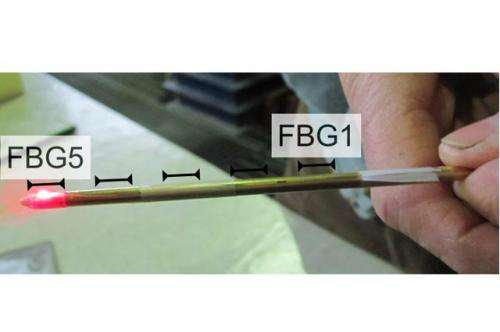
First produced in the 1990s, DTGs have superior strength and optical properties, however it is only recently that their commercial manufacture has become viable. "Our sensor design is based on the DTG fabrication process, allowing inscription of FBGs in a single fibre with higher density. It has 5 FBGs, each with 0.5 cm active length and 0.5 cm 'blank', allowing perfect labelling of the sensor positions," explained team member Dr Daniele Tosi. This provides a real-time estimation of the thermal dosimetry, point-by-point along the ablation axis.
DTG manufacture also doesn't require the fibre to be stripped, which maintains the fibre strength, allowing their use in vivo without external catheterisation, so the sensor can be mounted outside the RFTA needle to more directly sense the temperature of the tissue, rather than the needle itself.
"Multiple DTG arrays can be installed on a single ablation device. With respect to previous fibre-optic sensors, DTGs solve both the problems of unambiguous labelling of the sensor and robustness of the FBGs. It is a sensing structure suitable for short-term commercialisation as a hyperthermia sensor," said Tosi.
Increasing use
The team's goal is to have an array of sensors, mounted on multiple arms of an umbrella-shaped needle, as well as offering the surgeon the option of manually placing additional separate sensors around the treatment site. However, there are still challenges to address, chiefly, how to mount the sensor on the RFTA needle.
The mounting cannot use epoxy because of biocompatibility and high-temperature resistance issues. "Commercialization of the sensor for RFTA will involve integration of the sensor structure in the ablation device," said Tosi, and this type of sensor could allow RFTA to be used for even more types of tumours. "Quasi-distributed percutaneous temperature sensing could help expand RFTA use to tumours not commonly treated this way because of potential dangers; such as prostate cancer, where excess ablation can cause rectal or retro-urethral fistula. Temperature sensing in this context can act as a protection tool, detecting proximity of the temperature field to critical assets."
For the team, the bigger picture is the development of fibre-optic sensors to improve clinical outcomes of RFTA and the extension of its use as it is an outpatient procedure that is less invasive than other ablation options. But they see the potential for DTGs in medicine as being much wider than this, as Tosi explained: "FBGs in general, and DTGs in particular, have the potential to emerge as a mass market for medical devices: they are scalable, suitable for mass-production and, unlike many sensors, are plug & play."
More information: "Monitoring of radiofrequency thermal ablation in liver tissue through fibre Bragg grating sensors array" D. Tosi, et al. . Electronics Letters, Volume 50, Issue 14, 03 July 2014, p. 981 – 983, DOI: 10.1049/el.2014.0620 , Print ISSN 0013-5194, Online ISSN 1350-911X
Journal information: Electronics Letters
Provided by Institution of Engineering and Technology



















