August 12, 2013 report
Researchers mass produce reprogrammed T cells that target cancer cells
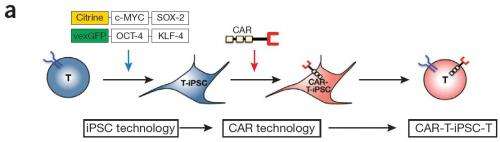
(Phys.org) —A team of researchers at the Memorial Sloan-Kettering Cancer Center has developed a method for mass producing T cells that have been reprogrammed using stem cell technology to target and destroy cancerous tumors. In their paper published in the journal Nature Biotechnology, the team describes how they collected isolated T cells, reprogrammed them into stem cells, added a gene marker, than reprogrammed them back into T cells that are able to target cells in cancerous tumors.
This new effort builds on research conducted this past March where a team held clinical trials that showed that genetically modified T cells could be used to target and destroy tumors (that came about due to lymphoblastic leukemia). Though successful, that effort resulted in a difficult to employ therapy. In this second-stage, the researchers developed a technique that allowed for mass producing reprogrammed T cells, thereby making the therapy more easily applicable.
To mass produce the cells, the researchers started by extracting T cells from a donor mouse. Those T cells were then modified to reprogram them into stem cells. Next, the researchers transferred gene information from a disabled retrovirus into the stem cells. The final step was reprogramming the stem cells back into T cells. Because they contained new gene information the newly minted T cells were capable of attacking cancer cells. Once created, the T cells were then nurtured into reproducing naturally—creating up to 1000 copies of themselves. Those cells were then injected back into the original donor mouse where they set to work destroying tumor cells.
The researchers note that the reprogrammed T cells are not really T cells in a technical sense—they're actually a new type of cell that closely resemble T cells, but have added capabilities. They add that their technique should also allow for the creation of different types of the T cell mimics allowing for targeting different types of cancer cells.
As with all such research, more studies will need to be conducted to learn more about the cells the team is creating before they can be tested in human trials. The researchers are optimistic, however, suggesting that their technique for treating cancer could be in general use as early as 2020.
More information: Generation of tumor-targeted human T lymphocytes from induced pluripotent stem cells for cancer therapy, Nature Biotechnology (2013) DOI: 10.1038/nbt.2678
Abstract
Progress in adoptive T-cell therapy for cancer and infectious diseases is hampered by the lack of readily available, antigen-specific, human T lymphocytes. Pluripotent stem cells could provide an unlimited source of T lymphocytes, but the therapeutic potential of human pluripotent stem cell–derived lymphoid cells generated to date remains uncertain. Here we combine induced pluripotent stem cell (iPSC)7 and chimeric antigen receptor (CAR)8 technologies to generate human T cells targeted to CD19, an antigen expressed by malignant B cells, in tissue culture. These iPSC-derived, CAR-expressing T cells display a phenotype resembling that of innate ?? T cells. Similar to CAR-transduced, peripheral blood ?? T cells, the iPSC–derived T cells potently inhibit tumor growth in a xenograft model. This approach of generating therapeutic human T cells 'in the dish' may be useful for cancer immunotherapy and other medical applications.
Journal information: Nature Biotechnology
© 2013 Phys.org















