Practicing medicine at the nanoscale: New approaches to drug delivery offer hope for new, more targeted treatments
Modern medicine is largely based on treating patients with "small-molecule" drugs, which include pain relievers like aspirin and antibiotics such as penicillin.
Those drugs have prolonged the human lifespan and made many life-threatening ailments easily treatable, but scientists believe the new approach of nanoscale drug delivery can offer even more progress. Delivering RNA or DNA to specific cells offers the promise of selectively turning genes on or off, while nanoscale devices that can be injected or implanted in the body could allow doctors to target drugs to specific tissues over a defined period of time.
"There's a growing understanding of the biological basis of disease, and a growing understanding of the roles certain genes play in disease," says Daniel Anderson, the Samuel A. Goldblith Associate Professor of Chemical Engineering and a member of MIT's Institute for Medical Engineering and Science and David H. Koch Institute for Integrative Cancer Research. "The question is, 'How can we take advantage of this?'"
Researchers in Anderson's lab, as well as many others at MIT, are working on new ways to deliver RNA and DNA to treat a variety of diseases. Cancer is a primary target, but deliveries of genetic material could also help with many diseases caused by defective genes, including Huntington's disease and hemophilia. "There are many genes that we think if we could just turn them off or turn them on, it could be therapeutic," Anderson says.
One promising avenue is RNA interference (RNAi), a naturally occurring process that allows cells to fine-tune their gene expression. Short strands of RNA called siRNA intercept and destroy messenger RNA before it can carry protein-building instructions from DNA to the rest of the cell. Scientists hope that by creating their own siRNA to target specific genes, they will be able to turn off genes that cause disease.
However, this potential has not yet been realized because of challenges in safely delivering siRNA to the right tissues and avoiding other tissues. Using viruses is one possibility, but is an option that carries some safety risks, so many researchers are now investigating synthetic delivery vehicles for genetic material.
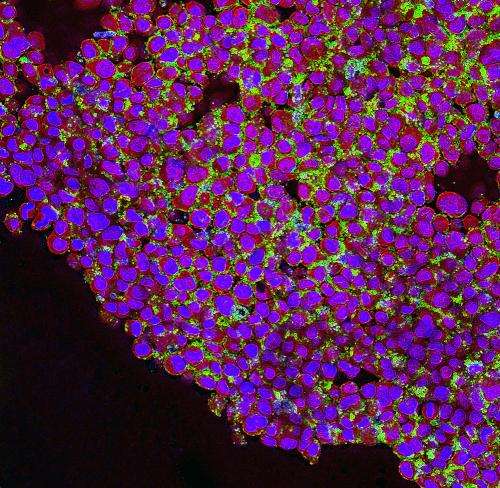
Anderson's lab is developing materials called lipidoids, fatty molecules that can envelop and deliver strands of siRNA. Studies have shown that these materials can effectively deliver RNA and shrink tumors in animals; MIT researchers are now working on developing them for human tests. These particles can deliver many RNA sequences at once, allowing researchers to target multiple genes. "A lot of these diseases, in particular cancer, are complicated and may require turning off multiple genes, or turning some genes off and some genes on," Anderson says.
Anderson is also using a technique called nucleic-acid origami to fold DNA and RNA into structures suitable for targeting cancer cells. Nucleic-acid origami, developed within the past few years, allows for extremely precise control over the location of every atom within a structure—something that is difficult to achieve with other types of nanoparticles, Anderson says.
In a 2012 study involving mice, Anderson showed that folded DNA nanoparticles tagged with folate accumulated in ovarian cancer cells, which express many more folate receptors on their surfaces than healthy cells.
Multipronged approach
Paula Hammond, the David H. Koch Professor of Engineering and a member of the Koch Institute, is also developing new materials for delivering both RNA and traditional drugs. Using her layer-by-layer assembly technique, she is creating nanoparticles that incorporate layers of multiple types of RNA, or combine RNA with a chemotherapy drug.
This multipronged attack could allow researchers to design treatments that cut off many of tumor cells' possible escape routes. "We're very interested in looking at combinations that would involve RNAi that knocks down the ability of cells to counteract chemotherapy attack," Hammond says.
Hammond's research in this area is now focused on cancer, but the approach could also lend itself to treating the inflammation produced by infectious diseases, she says. "With RNAi, the approach is fairly modular, and once you understand which genes you need to impact, you can work on targeting them," Hammond says.
Hammond's lab is also working on medical-device coatings that could secrete useful drugs, hormones or growth factors. One such project involves coating hip implants with layers that secrete bone growth factors. In studies with animals, she has shown that these coatings can promote the growth of natural bone, and stronger adhesion between hip implants and the body's own bone. If the work translates to human clinical use, it could allow hip implants to last longer and reduce the need for additional surgeries to replace the implants.
Hammond is also working on materials that promote wound healing by preprogrammed release of growth factors from bandages and dressings, and on ultrathin, transparent coatings for cataract-replacement lenses that release anti-inflammatory drugs.
Delivery and diagnostics
Michael Cima, the David H. Koch Professor of Engineering, and Robert Langer, the David H. Koch Institute Professor, both members of the Koch Institute, are working on nano- and microscale devices that can be implanted in the body to release drugs or diagnose disease.
Several years ago, Cima and Langer began working on an implantable chip that can dispense medicine inside the body, but which is controlled wirelessly from outside the body. In clinical trials last year, the company developing the chip for commercial use showed that it could reliably deliver precise doses of an osteoporosis medication that is normally given by injection.
The company developing the chip, MicroCHIPS Inc., is now shrinking the device and increasing the number of drug reservoirs on the chip (the version used in last year's trial had 20 such wells). That may enable the device to be used for much longer time periods—up to 30 years, Cima says. That would allow it to serve as an artificial gland, releasing hormones as necessary, he says, especially if a sensor could be incorporated to alert the chip when to release a dose.
Such a device could be useful for many endocrine diseases. "Diseases of growth, development and reproduction are all areas where there are significant unmet needs, or therapies that are very difficult to implement," Cima says.
Cima is also working on diagnostic devices that could help monitor tumor response to treatment, or detect whether someone has had a heart attack. His strategy is to take tests originally developed for in-vitro use (where a sample is removed from the body and tested in a lab), and instead put the sensing device inside the body. These diagnostic devices would be implanted in conjunction with a medical procedure.
For example, when cancer is suspected, a biopsy is done on a patient. Cima is now developing devices that could be implanted at the tumor site during the biopsy and later used to monitor oxygen level or acidity, both of which reveal important information about how the disease should be treated and whether the treatment is working.
Another sensor he developed uses magnetic nanoparticles, housed in an 8-millimeter disk implanted in the skin, to detect three proteins that are released during a heart attack. Anyone showing up at a hospital with chest pain is tested for those proteins, but results can appear inconclusive because the proteins are secreted at different times. The sensor, which is read using magnetic resonance imaging (MRI), could be implanted in patients known to be at high risk for a heart attack, making it much easier for doctors to determine if they have had one.
All of his projects, Cima says, are motivated by the desire to improve medical care for patients. "We're doing this because we can do some cool technology, but more importantly, we're doing it is because there's a clinically meaningful need," he says.
Provided by Massachusetts Institute of Technology
This story is republished courtesy of MIT News (web.mit.edu/newsoffice/), a popular site that covers news about MIT research, innovation and teaching.



















