This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Exploring how antibiotic-resistant bacteria become aggressive
Some strains of antibiotic-resistant bacteria that have recently acquired disease-enhancing genes may not behave as aggressively as expected, according to a Northwestern Medicine study recently published in Nature Communications.
Klebsiella pneumoniae, a common type of bacteria found in the intestines, can cause difficult-to-treat infections when introduced elsewhere in the body, as it's often resistant to traditional antibiotics. The bacterium poses the greatest risk to sick patients in hospital settings who are receiving treatment for other conditions, according to the Centers for Disease Control and Prevention.
New strains of Klebsiella pneumoniae that cause extremely aggressive infections even in healthy individuals have appeared in Asia in recent decades, according to the National Institutes of Health. While these aggressive strains remain susceptible to most antibiotics, there are concerns about emerging "convergent" strains that are both aggressive and antibiotic-resistant, said Alan Hauser, MD, Ph.D., vice chair of Microbiology-Immunology.
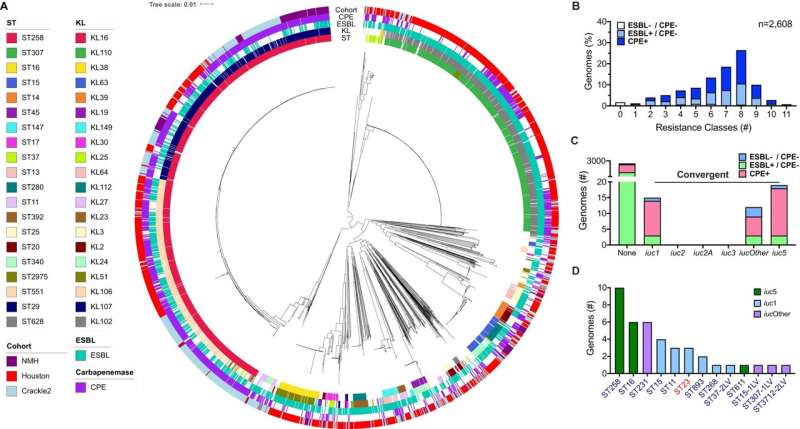
To identify these convergent strains, investigators led by Hauser analyzed the genomes of a large collection of the antibiotic-resistant bacteria taken from patients around the U.S.
"Recently, Klebsiella pneumoniae strains have been discovered that are both highly antibiotic resistant and hyper-virulent," said Hauser, who was senior author of the study. "Obviously, there's a lot of concern about these strains because not only do they cause these aggressive infections, but they're very difficult to treat. These strains are called convergent strains, and that's what the paper is about."
In the study, Travis Kochan, Ph.D., a postdoctoral scholar in the Hauser laboratory, and other investigators in Hauser's group sequenced the genomes of the 2,600+ strains and then narrowed their focus to 12 that had markers for being highly antibiotic-resistant and aggressive.
After performing long-read sequencing on the 12 strains, the scientists found that highly antibiotic-resistant forms of Klebsiella pneumoniae contain more plasmids—small, bacterial DNA molecules that can replicate independently of chromosomal DNA—than traditional strains, according to the study.
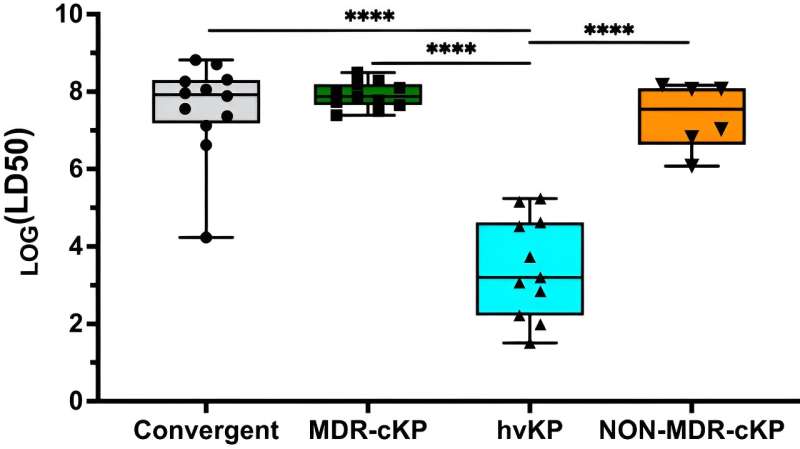
But when mice were infected with these strains, 11 of the 12 strains caused unexpectedly mild infections, Hauser said.
"What we found is that, with one exception, the convergent strains were no more virulent than their highly antibiotic-resistant counterparts," said Hauser, who is also director of Feinberg's Medical Scientist Training Program (MSTP). "This was surprising because the strains contained genes that were consistent with very high levels of virulence and the ability to cause aggressive infections. But 11 of the 12 did not cause aggressive infections."
Though one strain did produce an aggressive infection, the findings suggest that new convergent strains recently reported by a number of groups may not be as dangerous as physicians have feared.
"Certainly, we still need to be worried about these convergent strains; they are still a problem. They still have the potential to cause very serious and difficult-to-treat infections," Hauser said. "It's just that perhaps many of these convergent strains may not cause as severe infections as we originally thought."
More research is needed to understand why the genetics of Klebsiella pneumoniae do not always translate to the severity of the infection, Hauser said, and his laboratory will continue to study highly antibiotic-resistant strains of the bacteria.
"Our long-term goal is to come up with novel drugs that prevent Klebsiella pneumoniae from colonizing the GI tract by eradicating the strains in, for example, people in the intensive care unit who are at risk for serious infection," Hauser said. "If we can prevent an infection, then we don't have to worry about coming up with antibiotics to treat it, which is difficult with these strains because they're so antibiotic-resistant. That's the direction that my lab is going."
More information: Travis J. Kochan et al, Klebsiella pneumoniae clinical isolates with features of both multidrug-resistance and hypervirulence have unexpectedly low virulence, Nature Communications (2023). DOI: 10.1038/s41467-023-43802-1
Journal information: Nature Communications
Provided by Northwestern University




















