This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
One step closer to better drug therapies for tuberculosis
In ongoing research aimed at developing more effective treatments for tuberculosis (TB), University of Massachusetts Amherst microbiologists have identified a long-sought gene that plays a critical role in the growth and survival of the TB pathogen.
The discovery offers a potential target for drug therapies for a deadly disease that has few effective treatments and in 2021 alone sickened 10.6 million worldwide and caused 1.6 million deaths, according to the World Health Organization.
Published in the journal mBio, the research showed that the putative gene cfa encodes an essential enzyme directly involved in the first step of forming tuberculostearic acid (TBSA), a unique fatty acid in the cell membranes of mycobacteria. TBSA was first isolated from mycobacteria nearly 100 years ago but exactly how it's synthesized had remained elusive.
"There is a long history associated with this very fascinating fatty acid," says senior author Yasu Morita, associate professor of microbiology, in whose lab lead authors Malavika Prithviraj and Takehiro Kado carried out the research.
The experiments revealed how TBSA controls the functions of the mycobacterial plasma membrane, which acts as a protective barrier for the TB pathogen to survive in human hosts for decades.
"Cfa is directly involved in the formation of tuberculostearic acid and is also involved in the organization of the plasma membrane, and that all fell in place with our hypothesis," Prithviraj says.
The focus of research in Morita's lab is to identify ways to interrupt homeostasis of the thick and waxy cell envelope, which includes the plasma membrane, so the mycobacteria are unable to grow or vulnerable to attack. Prithviraj, a Ph.D. student, and colleagues performed cellular lipidomics to confirm what researchers have suspected for some 60 years.
"People have been very, very interested in understanding how this lipid is made and what it is doing in the cell," Morita says. "Malavika figured out that Cfa is the enzyme that makes this lipid, which is such a unique lipid that researchers have been pursuing this lipid as a diagnostic marker for TB."
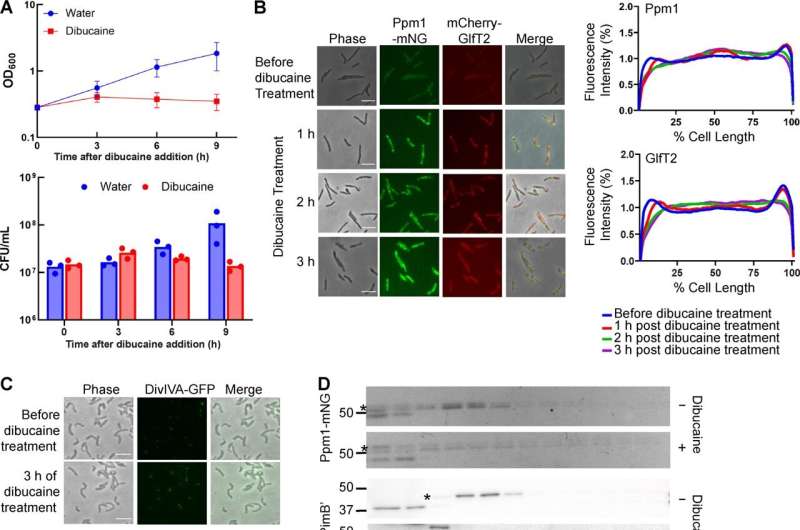
In previous experiments, the Morita lab had noted that plasma membrane domains found at polar regions of the cell were important for the growth of the mycobacteria.
"We were interested in understanding how this particular membrane domain is compartmentalized and organized in the bacteria," Prithviraj says. "We worked with a deletion strain of cfa and also a complement strain wherein we could add it back into the bacteria and check what exactly was its function."
The TB pathogen usually stays alive but dormant in the body for years or decades, thanks to its protective surface structure. Morita and his team work on a nonpathogenic model organism primarily to figure out what features of bacteria are needed for them to survive and grow.
The researchers found that TBSA also prevents "tight packing" inside the membrane. "If the membrane is too rigid, it cannot function properly, and so the membrane dynamics, or maintaining membrane fluidity, is very important," Morita says. "What we showed in this paper is that tuberculostearic acid is likely a very important molecular key for maintaining this proper fluidity."
The findings will help researchers take the next step toward developing new TB treatments.
"We would be interested in understanding the effects of the gene in TB infection and how Cfa might be helping the bacteria to survive in the human host" Prithviraj says. "If we find a way to disrupt the membrane fluidity maintenance, the cells cannot grow efficiently and would eventually die."
Morita adds, "There are many drugs used for treating TB, but there has been no previous demonstration that this particular aspect of mycobacteria physiology can be used as a direct target," Morita says. "This study is showing it could be."
More information: Malavika Prithviraj et al, Tuberculostearic Acid Controls Mycobacterial Membrane Compartmentalization, mBio (2023). DOI: 10.1128/mbio.03396-22
Journal information: mBio
Provided by University of Massachusetts Amherst




















