June 17, 2019 feature
Inducing an osteoarthritic (OA) phenotype in a cartilage-on-a-chip (COC) model
In an aging population, the social impact of osteoarthritis (OA) can dramatically increase to become the most common musculoskeletal disease. However, at present, therapies are limited to palliative treatments or surgical intervention alone, since disease-modifying OA (DMOA) drugs are scarce, primarily due to the absence of relevant preclinical models of the disease. As a result, tissue engineers and materials scientists aim to develop in vitro models for reliably predicting the efficacy of the requisite DMOA drugs.
To address this biomedical challenge, Paola Occhetta and an interdisciplinary research team in the departments of Biomedicine, Biomedical Engineering, Electronics, Information and Bioengineering in Switzerland developed a micro-physiological cartilage-on-a-chip model. Using the device, the scientists applied strain-controlled compression to the three-dimensional articular cartilage microtissue and recapitulated the mechanical factors involved in OA pathogenesis with an optimal 30 percent confined compression to induce OA traits in the lab.
Using only hyper-physiological compression (HPC) on the device, the scientists triggered a shift in cartilage homeostasis towards catabolism, inflammation and hypertrophy. Thereafter they obtained gene expression profiles similar to those observed in clinical osteoarthritic tissue. Occhetta et al. envision biomedical applications of the cartilage-on-a-chip device to screen clinical DMOA candidates in the near future. The results of the study are now published in Nature Biomedical Engineering.
Osteoarthritis is the most prevalent human musculoskeletal disease with its incidence expected to increase in an aging population to become a leading cause by 2020. Despite the prevalence, there is currently a lapse of available and effective pathology-reversing treatments, compelling medical research to develop new therapies and advanced strategies on bone tissue engineering. The complex and multifactorial etiology of OA can increase the difficulty in engineering a relevant preclinical model. While in vivo models provide a better reflection of the naturally occurring whole-joint disease, they are time consuming and costly. In vitro models are a highly desirable alternative, as they meet the 3R principles of replacing or reducing animal models and refining translational studies. However, the existing in vitro models of OA are too simplistic to encompass physiological features and predict the screening effects of drug candidates.
The main difficulty of reproducing cartilage tissue in vitro is due to the reliance of recapitulating the pathological disease either as a biochemical (cytokine-based) or mechanical (load-based) stimulation. Cytokine-based models rely on an overdose of inflammatory cocktails that induce a downstream effect, contrary to the actual OA environment found in vivo. In contrast, load-based models can trigger an OA-like response without supraphysiological doses of the biochemical stimuli.
Increasing evidence also correlates mechanical abnormalities such as obesity, trauma or joint misalignment to the onset of OA, classifying biomechanics as a key player disease progression. Load-based models are largely based on macroscale bioreactors to generate a pathological load response, yet they fail to fine tune the required microenvironmental stimuli. As an alternative, organs on chips devices are an emerging technology that can encapsulate organ functions at the microscale with unprecedented adherence to the pathophysiology in vivo for drug screening tests.
In the present work, Occhetta et al, developed a microscale system to reproducibly generate a human cartilage-on-a-chip (COC). For this, they used mechanical actuation to recapitulate the mechanical stimuli inherent in OA pathogenesis, using compression specifically as a mode of cartilage deformation. The bioengineers induced OA traits in the COC device, shifting matrix deposition and resorption balance towards catabolism to trigger a gene profile that correlated with clinical OA symptoms. The scientists used the device to test new disease-modifying OA (DMOA) candidates of anti-inflammation and anti-degradation in the present work.
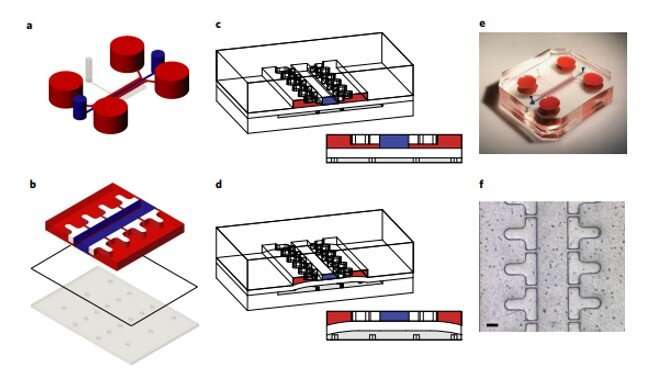
The device contained two chambers divided by a flexible membrane into an upper chamber hosting the 3-D micro-construct and a lower chamber as an actuation compartment realized with polydimethylsiloxane (PDMS) polymer. Based on a concept previously developed by the same research team, Occhetta et al. developed a COC device by:
- Confining a cell-laden prepolymer solution for the seeding and polymerization phases,
- Defining a length to control the mechanism of mechanical actuation.
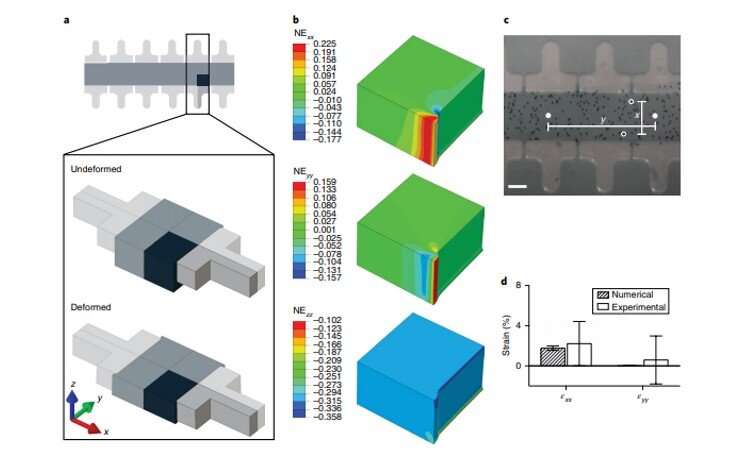
The scientists maintained the 3-D construct initially in a relaxed state, followed by designs to achieve 10 to 30 percent compression levels. They first tested the highest compression level using a finite element model (FEM) and used an enzymatically cross-linked matrix metalloproteinase (MMP) degradable poly (ethylene glycol) (PEG)-based hydrogel to mimic the 3-D microenvironment. The bioinspired hydrogel architecture mimicked the cartilage to exhibit largely nonlinear and strain-dependent behavior via interactions between the two material constituents of a solid matrix and an incompressible permeating fluid. They validated the numerical results experimentally to achieve the expected levels of mechanical actuation within the device.
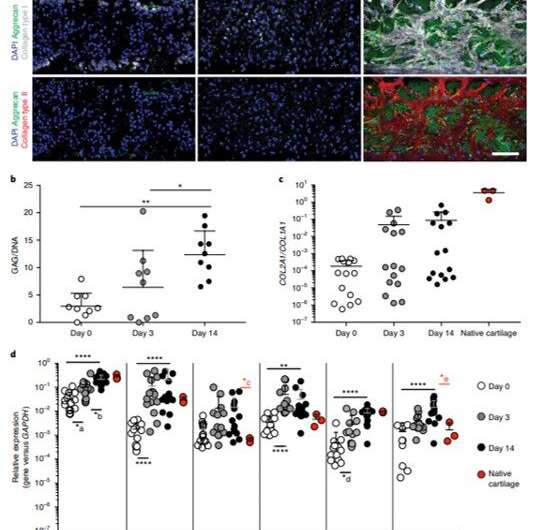
Occhetta et al. established the microscale device as a model of human COC using human articular chondrocytes (hACs) from healthy donors, embedded in the PEG gel. They obtained a cartilage micro-construct after 14 days of chondrogenic culture with geometric control for subsequent mechanical stimulation, which they verified using immunofluorescence assays and gene expression profiles. The scientists revealed high deposits of differentiated cartilaginous proteins that formed ECM rich collagen types I, II and aggrecan in the micro-construct. They similarly showed significantly increased articular cartilage-specific gene expression profiles at day 14 using qRT-PCR.
Using the established COC, the scientists applied mechanical stimulation through an electro-pneumatic actuation system at different levels of compression, for seven days. The induced mechanical patterns on the device resembled the biomechanics of a daily walk routine. The overall results of biochemical, molecular and mechanical assays showed that the hyper-physiological load conditions simulated in the COC triggered a loss of anabolic gene expression to mimic traits of OA. Similarly, Occhetta et al. investigated the impact of mechanical compression on catabolic and inflammatory profiles to suggest the onset of inflammation due to significant upregulation of a key pro-inflammatory cytokine interleukin 8 (IL-8) in the model.
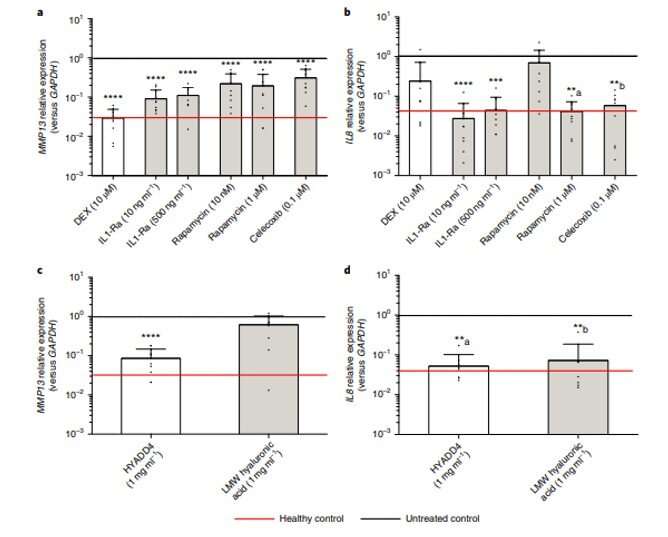
The hyper-physiological compression model also included the expression of several genes correlating to OA to match the gene expression profile of the disease. Suggesting that the model triggered the hypertrophic differentiation of hACs (human articular chondrocytes) towards transient chondrocytes. Occhetta et al. were able to regulate some of the genes by administering supraphysiological doses of anti-inflammatory drugs within the COC model.
In order to pharmacologically validate the OA COC model, the scientists first removed both serum and transforming growth factor beta (TGF-β) in the medium to avoid masking the pharmacotherapeutic effects. They selected two drugs; interleukin-1 receptor antagonist (1L-1Ra) and rapamycin. In the COC model, rapamycin, which is a mammalian target rapamycin (mTOR) inhibitor, specifically reduced the expression of MMP13 gene (matrix metallopeptidase 13) and only had a significant effect on IL-8 when administered at the highest dose. The scientists also tested a pharmaceutical candidate currently in commercial development and further verified the efficacy of the new COC model, consistent with previous preclinical and clinical reports.
In this way, Occhetta and co-workers developed and established a microscale system within a PEG-hydrogel-based 3-D microenvironment, which included a mechanical actuation system. They allowed defined levels of confined compression in the setup to mimic the biomechanics of OA in an in vitro model of the disease. Using the device as a proof-of-principle drug screening tool, the scientists tested DMOA (disease modifying osteoarthritic) drugs and potential pharmaceutical candidates in the lab. Occhetta et al. aim to optimize the device to reproduce structural and functional cues to study the biomechanical response of tissues such as bone under pathophysiological conditions and therapeutic intervention in healthcare.
More information: Paola Occhetta et al. Hyperphysiological compression of articular cartilage induces an osteoarthritic phenotype in a cartilage-on-a-chip model, Nature Biomedical Engineering (2019). DOI: 10.1038/s41551-019-0406-3
Johannes WJ Bijlsma et al. Osteoarthritis: an update with relevance for clinical practice, The Lancet (2011). DOI: 10.1016/S0140-6736(11)60243-2
Eric W. Esch et al. Organs-on-chips at the frontiers of drug discovery, Nature Reviews Drug Discovery (2015). DOI: 10.1038/nrd4539
Journal information: Nature Biomedical Engineering , The Lancet , Nature Reviews Drug Discovery
© 2019 Science X Network





















