New strategy may drop cancer's guard
A drug used now to treat Type 2 diabetes may someday help beat breast and ovarian cancers, but not until researchers decode the complex interactions that in some cases help promote tumors, according to Rice University scientists.
Rice bioscientist Daniel Carson and alumna Micaela Morgado researched thiazolidinediones, small molecules used to fight diabetes, that can halt the expression of glycoproteins that make up the protective mucus that lines cells and organs in the body. These mucus cells are manipulated by tumors to keep them safe from chemotherapy and the immune system.
But there are problems to be solved before the drug can be used to fight cancer, Carson said, including the fact that small doses appropriate for diabetes treatment actually increase cancer risk for patients with diabetes. The drug they studied, rosiglitazone, shows promise only if it can be delivered in large-enough doses and directly to tumors, he said.
The work will appear in the January issue of the Journal of Cellular Biochemistry.
"My lab is interested in the class of very high-molecular-weight glycoproteins that absorb water and cover and protect the surfaces of your cells," Carson said. "These mucins perform a very important protective function, lining your mouth, your glandular structures and your gastrointestinal tract, essentially acting like Teflon for those surfaces.
"But tumors have learned a trick," he said. "Instead of keeping mucins on one end of a cell, where they would normally protect it from the external environment, they start putting mucins all over their surfaces. Cells of the immune system that kill tumors have to make contact with the cancer cell's surface, but when they have these big barrier molecules on the surface, they're protected.
"If we can intervene in patients and reduce mucin levels, maybe the host immune system can do its job and kill the tumors," Carson said.
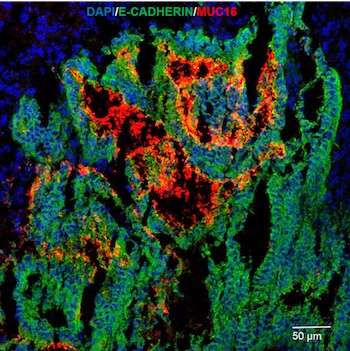
The lab studied the effects of one thiazolidinedione, rosiglitazone, on a glycoprotein known as MUC16 that protects breast and ovarian cancer cells. Another, pioglitazone, was the focus of a recent Rice breast cancer study, and Carson's lab previously studied the effects of rosiglitazone on another glycoprotein, MUC1.
"MUC16 wound up being particularly interesting because it's also known as CA125, which is the gold standard marker for ovarian cancer," he said. "Women are routinely monitored for CA125 levels that normally are found at very low levels in serum. If you have certain tumors, these cancer cells begin to release fragments of CA125."
Carson said doses of rosiglitazone fed to cancer cell lines in the lab shut down the production of glycoproteins by interfering with the actions of cytokines that trigger the cells' protective response and elevate MUC16 production.
"It turns out the tumor microenvironment is rich in these cytokines," he said. "You would think these pro-inflammatory mediators would be a good thing because they enhance the immune response to the tumor. But, in fact, they also enhance the tumor's protective response."
He said stopping production of MUC16 for even a couple of days might be enough to breach the protective shield and allow immune cells to begin the destruction of a tumor. "If you could shut down synthesis by 90 percent or more, which is achievable with these drugs, within two days you have enough reduction to remove the tumor's protective coating.
"There's nothing here we can take to a clinic yet," Carson said. "We learned about ways to intervene and reduce the expression, but we either need better drugs that can do it at much lower, pharmacologically achievable levels, or we need to have a way to target drugs so we can get tumor-specific, superphysiological concentrations that would achieve the goal.
"The upside is that these drugs are already FDA approved," he said. "If we can repurpose them, we don't have to go through the same duration of regulatory process required to use them for cancer therapy."
More information: Micaela Morgado et al. PPARγ Modulation of Cytokine-Stimulated MUC16 (CA125) Expression in Breast and Ovarian Cancer-Derived Cells, Journal of Cellular Biochemistry (2017). DOI: 10.1002/jcb.25622
Journal information: Journal of Cellular Biochemistry
Provided by Rice University



















