How antibiotics spread resistance
Bacteria can become insensitive to antibiotics by picking up resistance genes from the environment. Unfortunately for patients, the stress response induced by antibiotics activates competence in microorganisms, the ability to take up and integrate foreign DNA. Microbiologists from the University of Groningen (UG) and the University of Lausanne have now described a new mechanism by which Streptococcus pneumoniae can become competent, and why biofilms may be important in this process. Their results were published in Cell Reports on November 27.
UG Ph.D. student Jelle Slager first described the mechanism of competence four years ago. Subsequently, his colleague Arnau Domenech, a team member from the Veening lab at the University of Lausanne, who is the first author of the Cell Reports paper, screened a large number of clinically relevant substances for their ability to induce competence. Two drugs stood out: aztreonam and clavulanic acid, which are both used to fight infections. "But when we looked closer, they didn't affect competence through a known mechanism," says Slager. "So we investigated what was going on."
Cell division
Competence is induced through the release of competence stimulating peptide (CSP). Cells secrete this peptide when they experience stress, for example, when they are challenged with certain antibiotics. Only when the CSP concentration around them reaches a certain threshold do the cells become competent. "This is a process called quorum sensing, which elicits a response once enough cells are affected." As CSP is secreted into the environment, all cells become competent at more or less the same time.
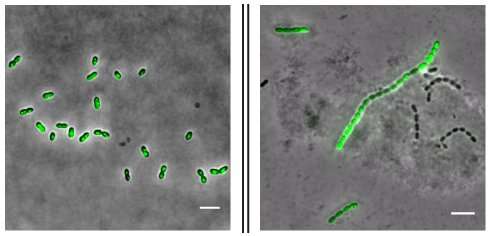
However, something different happened with the Streptococcus pneumoniae cells used in this study. Slager says, "As these cells divide, they normally form mother-and-daughter pairs. But in response to these two drugs, they start forming longer chains, as the cell division mechanism is affected by the drugs. When cells in these chains secrete CSP, the local concentration is higher than when pairs of cells swim freely in the medium. This means the local threshold for quorum sensing will be reached sooner for the cells in these chains.
Biofilm
Slager says, "Through this mechanism, groups of cells become competent at different times. So rather than a synchronized 'pulse' of competence in all the cells, which we normally see, we now have competent cells present for an extended period of time." An interesting aspect of this finding is that bacterial cells do not freely float in the body, as in these laboratory experiments, but are usually incorporated within a biofilm. Bacteria produce these biofilms by excreting sticky molecules, which provide them with protection against the immune system, for instance.
"In these biofilms, the cells are packed much more closely together, which means that competence is probably regulated by local quorum sensing, just like in our experiments," says Slager. "In fact, as was recently discovered, a gene that stimulates biofilm formation is activated together with other competence-induced genes." The first conclusion from this study is that standard laboratory experiments in which free-swimming bacteria are grown in flasks full of culture medium are different from the clinical situation, in which they would grow in a biofilm. Furthermore, drugs that lead to chain formation, like aztreonam and clavulanic acid used in this study, will thereby increase the spread of antibiotic resistance genes.
Will this have any clinical implications? Not directly, says Slager. "This study primarily increases our fundamental knowledge about the spread of antibiotic resistance genes. And it tells us more about how cells communicate through quorum sensing. But maybe, in the long run, this knowledge could be used to disturb this communication and perhaps reduce the development of resistance."
More information: Arnau Domenech et al, Antibiotic-Induced Cell Chaining Triggers Pneumococcal Competence by Reshaping Quorum Sensing to Autocrine-Like Signaling, Cell Reports (2018). DOI: 10.1016/j.celrep.2018.11.007
Journal information: Cell Reports
Provided by University of Groningen





















