'Human touch' nanoparticle sensor could improve breast cancer detection
(Phys.org) —University of Nebraska-Lincoln scientists have developed a nanoparticle-based device that emulates human touch and that could significantly enhance clinical breast exams for early detection of cancer.
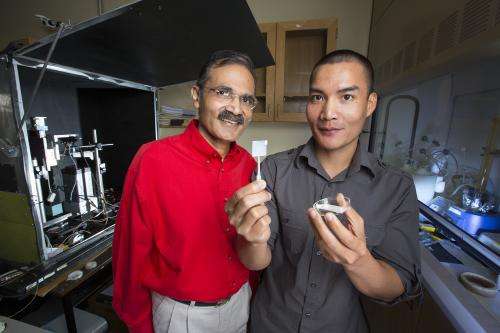
In a newly published article in the journal ACS Advanced Materials & Interfaces, researchers Ravi Saraf and Chieu Van Nguyen describe a thin-film sensor that can detect tumors too small and deep to be felt with the fingers.
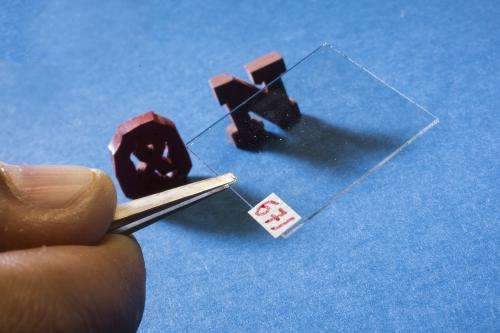
In research funded with a grant from the National Institutes of Health, Saraf and Nguyen perfected a thin film made of nanoparticles and polymers, which when pressed against the skin creates changes in electrical current and light that can be captured by a high-quality digital camera.
The film, just one-60th the thickness of a human hair, is a sort of "electronic skin" able to sense texture and relative stiffness.
Using a silicone breast model identical to those used to train doctors in manual breast exams, the researchers ued the film to successfully detect tumors as small as 5 millimeters, hidden up to 20 millimeters deep. The technology also would allow improved detection for skin cancer.
Saraf, a professor of chemical and biomolecular engineering, said he envisions a stethoscope-like device that a doctor would press across a patient's chest to image the buried palpable structure. It could be used by family doctors during routine patient examinations or by physicians serving remote regions of the world.
The film is easy to manufacture using readily available industrial processes and remains stable for months, he added.
"A tool like this could be interfaced with a laptop to provide high-quality screening capability to save lives in poor countries in remote parts of the world," Saraf said.
The next step, Saraf said, is to acquire funding to build a prototype device.
"We have enough know-how now. We can start building this device today," he said.
He estimated a prototype would cost about $1.5 million and take about a year to build.
In clinical breast examination, or CBE, doctors manually examine the breast for abnormalities and use their hands to palpate the tissue in search of lumps. Though it may seem low-tech compared to mammograms, magnetic resonance imaging and ultrasound, CBE is an important cancer-screening tool.
Mammograms, which identify lumps by their density compared to breast tissue, are less effective with young women and those with dense and vascular breasts. MRI and ultrasound are more sensitive than mammography, but are too expensive for use as a screening tool.
Yet the challenge with CBE is the lack of a visual record to compare with previous examinations to aid in diagnosis. Also, manual breast exams typically don't find lumps until they are 21 millimeters big, while the American Cancer Society reports a 94 percent survival rate if breast cancer is diagnosed when tumors are diagnosed at less than 10 millimeters.
Saraf said the thin-film tool would have at least three advantages to a manual breast exam performed by a physician: It is more sensitive; it creates an image of the lump that can be included in the patient's records; and it provides faster results than other imaging technology.
"Other tests, such as mammogram and MRI, require a nerve-wracking wait until the results are reported," Saraf said. "This is more like an ultrasound, providing immediate results without radiation and not as uncomfortable as a mammogram."
Other devices have attempted to do this, but their image quality is poor and they cannot determine a lump's shape, often a key to determining whether it is cancerous.
An early version of the technology, reported in 2006, was able to detect differences in surface texture. The latest version measures comparative stiffness. Typically, malignant lumps are at least nine times as stiff as the surrounding breast tissue.
Saraf said the key to success was finding the right balance of sensitivity and pressure: If too much pressure is required, the tool would cause patient discomfort. Yet if the film is too sensitive, it would create a saturated image and prevent visualization of a deeper embedded mass.
Provided by University of Nebraska-Lincoln



















