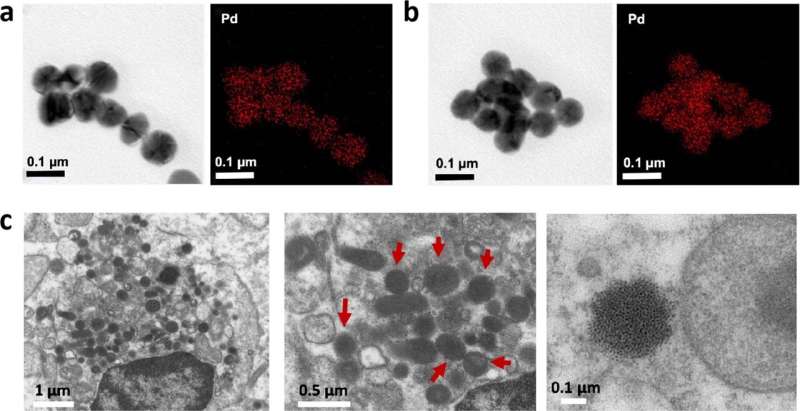
EM images of PdL nanoparticles detected in DMEM, blood and tumor site. (a, b) TEM and EDX element mapping images of nanoparticles detected in DMEM (10% FBS) and in the blood of mice 5 min after treatment with PdL. (c) EM images at different magnifications of slices of A375 tumors in mouse xenografts 12 h after intravenous tail injection of PdL. Nanoparticles are indicated by red arrows. Credit: Nature Chemistry (2023). DOI: 10.1038/s41557-023-01199-w
Chemotherapy that does not harm the body, but effectively fights cancer cells: that is the goal of chemist Sylvestre Bonnet and his team. During his Ph.D. research, chemist Xuequan Zhou brought that goal a little closer. He developed molecules that, upon injection into the bloodstream, self-assemble into nanoparticles that accumulate in the tumor. Targeted irradiation with visible light then attacks the tumor. The research has now been published in Nature Chemistry.
"Conventional anti-cancer drugs often do not differentiate enough between good and bad cells," Bonnet explains. "They kill them both." The researchers have come up with a solution to this problem: nanoparticles that target the tumor and only become active under the influence of visible light. "This anticancer phototherapy allows doctors to treat a specific part of the body without damaging the rest. It is already in use in several hospitals."
Molecules that form nanoparticles by themselves
Until now, chemists had to first attach the chemotherapy drugs to nanoparticles in the lab. Doctors then administered them by injection into the patient's bloodstream. Conjugation to the nanoparticles helped the chemotherapy find the tumor. Zhou's drug works slightly differently. "The lab work is no longer necessary," he says. "You can administer the molecules directly. Once in the blood, nanoparticles then form all by themselves."
And that has several advantages, says Zhou. "First, it saves a lot of work and preparation time. But in addition, it is also safer and more effective." Making nanoparticles in the lab is complicated: it always creates a mix of particles with varied sizes and therefore different properties. It is difficult to precisely determine the composition of that mix. So you are never 100% sure how these particles are going to behave in your body.
Zhou says, "With a molecule, this is more straightforward: when you make molecules, chemical analysis allows you to determine whether they are pure." Bonnet adds, "If you then inject these molecules into the blood, the resulting nanoparticles are all really similar. That is because the body processes those molecules all in the same way."
Xuequan's molecule is a so-called palladium complex—a molecule with a metallic core made of palladium. Normally, the palladium atom is connected to four nitrogen atoms, but Zhou replaced two of those nitrogen atoms with carbon atoms. When irradiated with green light, the palladium complex gains extra energy. That extra energy causes the complex to transfer electrons to the oxygen molecules (O2) already present in the irradiated cells. This mechanism creates a reactive oxygen species that kills cancer cells.
In 2020, Zhou also made a cancer drug with self-assembling properties. "However, this new molecule is one step further," he says. "By binding not one but two carbon atoms to the metal, the drug is now activated under green light, instead of blue." Green light allows better penetration into body tissue and is therefore much more useful for therapy in mice. "Our ultimate goal is a drug that works under infrared light," says Bonnet. "That light would allow even deeper penetration. It would allow us to fight larger tumors deep inside the body of human patients."
This new study followed a better, clinically more relevant approach. In the first study, Zhou and his colleagues injected the drug directly into the tumor. "This time we went a step further and looked in mouse models where the drug was injected into the bloodstream," he says. "After all, this is also how it would be done in hospitals. We wanted to know whether the drug nanoparticles would survive the conditions in the body. And fortunately, that was the case."
Zhou's molecule proved to be very effective. "Ten percent of the administered drug reaches the tumor," says Bonnet. "Out of every 100 molecules we administer, ten arrive at the destination. For many nanomedicines, that percentage is much lower. A study a few years ago showed that the average is only 0.7%."
How exactly is this possible? Molecules that form nanoparticles by themselves? "We don't exactly know that ourselves either," Bonnet admits. "We know palladium is critical, and Xuequan discovered that proteins in the blood probably play a role as well. If those proteins are missing, the nanoparticles keep growing and become so big that they eventually no longer stay in solution. It hence seems that the proteins limit the growth of the nanoparticles, but we cannot yet precisely tell how. We know it is effective. That's the most important thing. But why it does work so well? That's what further research will have to show."
More information: Xue-Quan Zhou et al, In vivo metallophilic self-assembly of a light-activated anticancer drug, Nature Chemistry (2023). DOI: 10.1038/s41557-023-01199-w
Journal information: Nature Chemistry
Provided by Leiden University