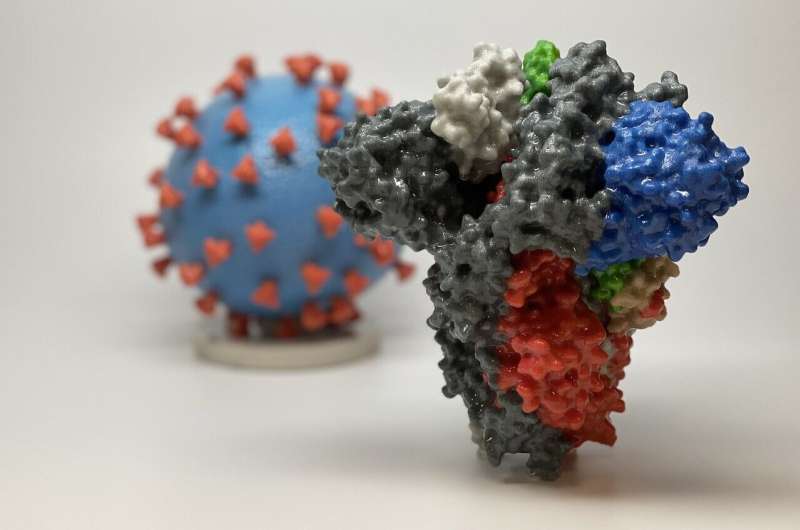
3D print of a spike protein of SARS-CoV-2, the virus that causes COVID-19—in front of a 3D print of a SARS-CoV-2 virus particle. The spike protein (foreground) enables the virus to enter and infect human cells. On the virus model, the virus surface (blue) is covered with spike proteins (red) that enable the virus to enter and infect human cells. Credit: NIH
Coronaviruses are slippery, and that makes it hard to create effective vaccines that provide long-term protection. Now, University of Connectiut (UConn) researchers have developed a new way to model the spike protein of the virus and test its binding to antibodies. That could give scientists a firmer grip on the virus that causes COVID-19.
By now, the majority of adult citizens in the US have been vaccinated against COVID, and many have had booster shots as well. Despite this, about 30% of hospitalized COVID patients in Connecticut are fully vaccinated. Although there are several different COVID vaccines in use around the world, none of them provides long-term, durable protection against the virus.
The problem is the coronavirus's spike protein. The spikes coat the virus, and are so wiggly and flexible that they slip through the clutches of antibodies like a weasel through a wedding ring. Without a firm grasp on the spike, the immune system cannot make good antibodies. And without good neutralizing antibodies, the immune system's memory of the virus is too fuzzy to last.
"It's kind of out-of-focus. Anything out of focus is hard to grasp, hard to understand, and hard to grab," says Paulo Verardi, a pathobiologist in UConn's College of Agriculture, Health and Natural Resources.
Verardi gave several lectures about the coronavirus early in the pandemic as part of "The COVID-19 Pandemic: Impacts on Health, Business, and Society," the largest and most popular class ever given at UConn, and many faculty members took it. Anna Tarakanova, a computational biophysicist and assistant professor of mechanical engineering, was one of them. She is an expert at modeling dynamic proteins. She spoke with two of her graduate students, Genny Kunkel and Mohammad Madani, and they had an idea. What if they modeled the spike protein, figured out how it moved when it interacted with the immune system, and then froze it in just the right position for the immune system to get a grip on it?
Tarakanova reached out to Verardi, and he liked the idea. Although all current COVID vaccines approved in the US use stabilized versions of the spike protein, no one knows if there are better or worse positions for the immune system to use as a template. Tarakanova's team could figure that out. UConn biochemist Simon White joined the team as well.
Their first paper, describing which parts of the spike protein flex, how mutations affect that flexibility, and how it all affects antibodies' grip, was published in the Biophysical Journal on Dec. 21. They also produced video clips of how the spike protein moves.
"We are actively building models of some of the emerging natural variants like delta, lambda, and omicron to see how this evolves," says Tarakanova.
They want to see how each variant interacts with antibodies, and eventually use that knowledge to make the best possible version for antibodies to fix on—so that the world has a vaccine against COVID that works for the long term, and doesn't require a booster every six months.
More information: Genevieve Kunkel et al, Modeling coronavirus spike protein dynamics: implications for immunogenicity and immune escape, Biophysical Journal (2021). DOI: 10.1016/j.bpj.2021.11.009
Journal information: Biophysical Journal
Provided by University of Connecticut