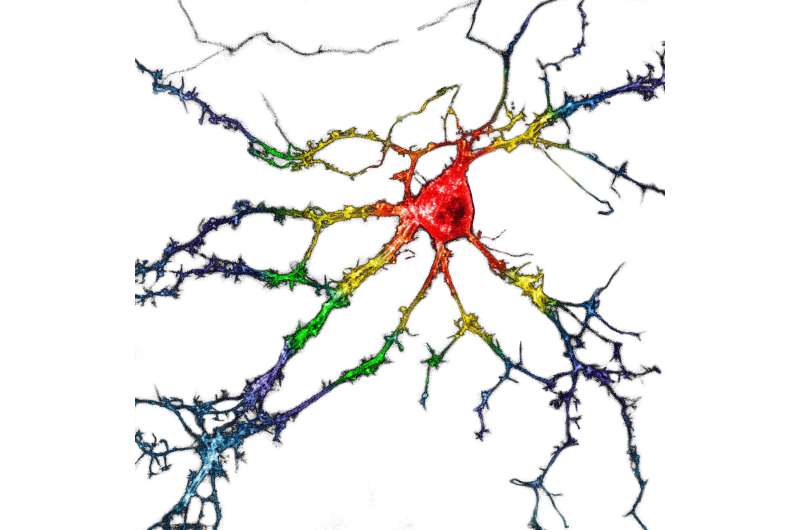
A representative image of cultured dissociated hippocampal neurons transiently expressing psychLight1 and psychLight2. Scale bar, 20 mm. Credit: Calvin Ly
Psychedelic drugs have shown promise for treating neuropsychiatric disorders such as depression and posttraumatic stress disorder. However, due to their hallucinatory side effects, some researchers are trying to identify drugs that could offer the benefits of psychedelics without causing hallucinations. In the journal Cell on April 28, researchers report they have identified one such drug through the development of a genetically encoded fluorescent sensor—called psychLight—that can screen for hallucinogenic potential by indicating when a compound activates the serotonin 2A receptor.
"Serotonin reuptake inhibitors have long been used for treating depression, but we don't know much about their mechanism. It's like a black box," says senior author Lin Tian, an associate professor in the Department of Biochemistry and Molecular Medicine in the School of Medicine at the University of California, Davis. "This sensor allows us to image serotonin dynamics in real time when animals learn or are stressed and visualize the interaction between the compound of interest and the receptor in real time."
Tian's lab joined forces with the lab of David E. Olson, an assistant professor in the Department of Chemistry at UC Davis, whose lab is focused on drug discovery. "This paper was an exceptionally collaborative effort," says Olson, a co-author on the study. "My lab is really interested in the serotonin 2A receptor, which is the target of both psychedelic drugs and classic antipsychotics. Lin's lab is a leader in developing sensors for neuromodulators like serotonin. It just made perfect sense for us to tackle this problem together."
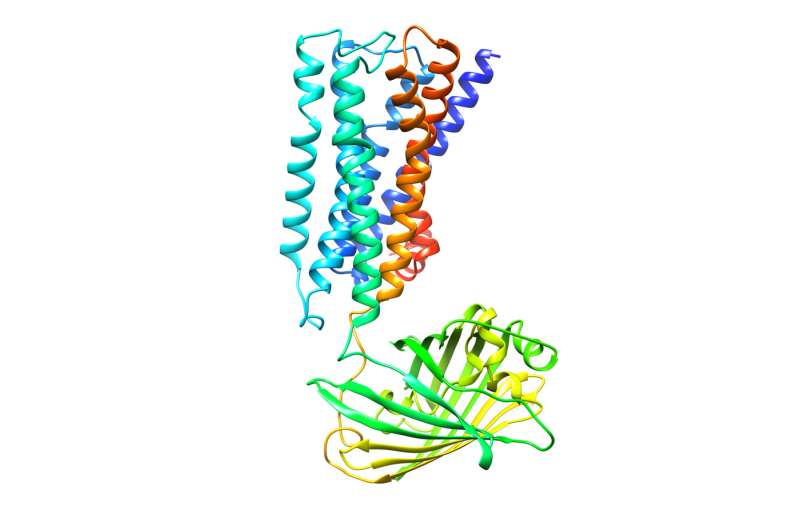
A simulated structure of psychLight consisting of 5-HT2AR (gray), a linker (magenta) and a cpGFP (green)--white background. Credit: Dong, Ly, and Dunlap et al.
Experts believe that one of the benefits of using psychedelic drugs over existing drugs is that they appear to promote neural plasticity—essentially allowing the brain to rewire itself. If proven effective, this approach could lead to a drug that works in a single dose or a small number of doses, rather than having to be taken indefinitely. But one thing that researchers don't know is whether patients would be able to gain the full benefit of neural plasticity without undergoing the "psychedelic trip" part of the treatment.
In the paper, the investigators report that they used psychLight to identify a compound called AAZ-A-154, a previously unstudied molecule that has the potential to act on beneficial pathways in the brain without hallucinogenic effects. "One of the problems with psychedelic therapies is that they require close guidance and supervision from a medical team," Olson says. "A drug that doesn't cause hallucinations could be taken at home."
The serotonin 2A receptor, also known as 5-HT2AR, belongs to a class of receptors called G protein-coupled receptors (GPCRs). "More than one-third of all FDA-approved drugs target GPCRs, so this sensor technology has broad implications for drug development," Tian says. "The special funding mechanisms of BRAIN Initiative from the National Institutes of Health allowed us to take a risky and radical approach to developing this technology, which could open the door to discovering better drugs without side effects and studying neurochemical signaling in the brain."
More information: Cell, Dong et al.: "Psychedelic-inspired drug discovery using an engineered biosensor" www.cell.com/cell/fulltext/S0092-8674(21)00374-3 , DOI: 10.1016/j.cell.2021.03.043
Journal information: Cell
Provided by Cell Press