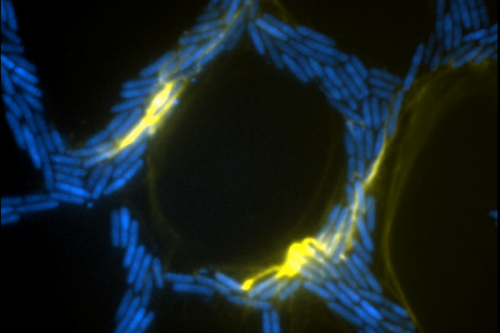
Extracellular DNA (yellow) in biofilms of the bacteria Pseudomonas aeruginosa organising traffic flow.
Ground-breaking research by Australian scientists has revealed new insights into how life-threatening bacteria colonise medical devices that are implanted in the human body.
The break throughs could help tackle antibiotic resistant infections that develop in groups of microorganisms where cells stick to each other on a surface, otherwise known as biofilms.
Biofilms are a significant threat to human and animal health because they are notoriously resistant to antibiotic treatment and immune defences. They are responsible for many chronic and recurring infections that occur around implanted medical devices.
Research published today in the prestigious journal Proceedings of the National Academy of Sciences (PNAS) by UTS Associate Professor Cynthia Whitchurch, used advanced microscopy techniques, including the next generation imaging system OMX Blaze, and sophisticated computer vision analysis to explore how bacterial biofilms spread. Associate Professor Whitchurch is leading a team of researchers from the UTS ithree institute, the UTS School of Mathematical Sciences, Monash University, University of Melbourne and CSIRO.
Studying the bacteria Pseudomonas aeruginosa, a pathogen that can cause respiratory disease and often causes infections when things such as catheters are inserted, has helped the team deduce how individual cell movements are co-ordinated and how intricate networks of interconnected trails are formed during biofilm expansion.
"This research reveals how co-ordination between individual bacteria can lead to complex group behaviour to enable biofilm expansion on a surface" says Associate Professor Whitchurch.
The researchers discovered that groups of bacteria build and migrate along a "furrow" on a surface – much like a well-trodden path across a grassy field. The team also discovered that extracellular DNA (eDNA) acted not as coding molecules but as a structural 'rope' that helped guide the transit of the bacteria.
What they discovered, in effect, was a traffic management system similar to signalling on a railway track that ensured a smooth flow of bacterial cells down the line towards the front of an expanding biofilm. eDNA also acted as glue, binding groups of bacteria together and forming 'bulldozers' that forged the furrows.
Through its ithree institute, UTS has invested in world leading imaging facilities alongside state-of-the-art genomic, bioinformatics and proteomic facilities.
The ground-breaking research demonstrated how such investment in world class facilities in NSW was advancing science as well as paving the way for its application to new medical discoveries, said Director of the ithree institute Professor Ian Charles.
"With the rise of resistant superbugs, we desperately need to find new ways to combat infectious diseases and I am confident that our research will make a contribution to that urgent quest" said Professor Charles.
The ithree institute is pioneering the use of OMX 3D SIM super resolution microscopy to advance the understanding of infectious disease. It is the world's first commercial site for the next generation DeltaVision OMX Blaze super resolution imaging system – a device developed and manufactured in the United States by Applied Precision, a GE Healthcare Company. It is capable of capturing real-time multiple colour images of interactions between microorganisms and living cells.
More information: Self-organization of bacterial biofilms is facilitated by extracellular DNA, www.pnas.org/cgi/doi/10.1073/pnas.1218898110
Journal information: Proceedings of the National Academy of Sciences
Provided by University of Technology, Sydney