Using interdisciplinary tools to find cure for human herpes virus
Human herpes virus, commonly known as herpes simplex virus 1 and 2 (HSV-1 and HSV-2), is like that friend who ends up crashing on your couch and never leaves.
Most of the time he lurks in the background, relatively innocuous but for the annoying thought of his presence. But occasionally he comes out of the shadows and ends up in the way in your kitchen at mealtime, uninvited and naturally wanting a little something for himself. Later he interrupts an intimate moment with a perfectly timed and inopportune knock at your bedroom door; and as time drags on, he generally spoils your good times by managing to be everywhere you wish he wouldn't be at precisely the wrong moments.
But unlike your couch-crashing "friend," you can't just put herpes out on the street and be done with it.
And worse yet, the Centers for Disease Control and Prevention estimate that, in the United States alone, herpes infects more than three-quarters of a million new people every year.
Moriah Szpara, assistant professor of biochemistry and molecular biology at Penn State and researcher at the Huck Institutes of the Life Sciences, aims to find a cure for the disease.
"Herpes simplex virus type 1 is fairly ubiquitous around the world," she says. "About 70 percent of all adults have seropositivity, meaning that they have signs of exposure to this virus in their bloodstream, and a fraction of those people suffer cold sores or genital sores—depending on the site of introduction—periodically for the rest of their lives."
Beyond being a simple, periodic annoyance, herpes sometimes exhibits hypervirulence: running amok in its host and causing blindness, aseptic meningitis (inflammation of the protective membranes covering the brain and spinal cord), or encephalitis (swelling of the brain). The latter two conditions can be fatal.
In fact, HSV-1 is the leading cause of infectious blindness in the United States and is the main cause of sporadic, fatal encephalitis. Because the drugs currently available to treat HSV treat only the virus's active, replicating phase and associated symptoms (for example, oral and genital sores), they do not affect its latency in neurons, which is what allows herpes to infect its host for life.
"In a very small number of cases that we don't understand the reason for, the virus can progress into the central nervous system and cause encephalitis," says Szpara, who is also a faculty member of the Bioinformatics and Genomics graduate program. "Because we don't know why it happens, we can't predict it and we can't stop it. Right now, the infection is permanent, and that's the biggest public health issue surrounding herpes—it's a dangerous virus, it's not benign, it's not friendly, and the infection will never go away."
Interdisciplinary approach
Early in her career, Szpara (pronounced like the tiny songbird, but ending with an "ah" instead of an "oh") is already leading the way in several important areas of human herpesvirus research.
Although a neurobiologist and virologist by training, Szpara has pioneered the use of comparative genomics for analyzing variation in HSV—variation that is key both to understanding the genetic factors that contribute to virulence and ultimately to developing a vaccine or a cure for the virus.
"The way we fix the problems caused by herpes is by understanding what the virus is doing in neurons," Szpara says. "That thing you see on your skin is a dead-end where the virus is jumping ship to get to the next person. The place where the virus hides is in your neurons, and it doesn't kill those neurons—it will kill your skin cells, but it uses your neurons as its home base. So that's where I come in: I'm a virologist and a neurobiologist with a toolbox in comparative genomics.
"As a neurobiologist, it's my job to figure out what the weak link is in neurons. And if I can't find it there, then I hope that by using comparative genomics to survey the different viruses circulating out there—since not everybody's virus is the same—that we'll find a weak link there. If we could find out what makes one virus worse than another, we might be able to find a way to disable the ones that are really virulent, or maybe we'll find one that's really weak that can be used to immunize people."
Postdoc to present day
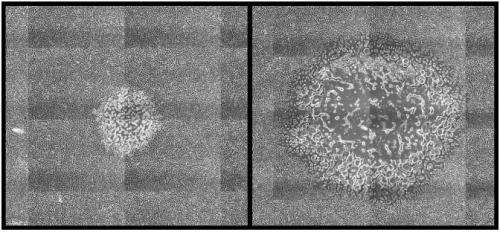
While pursuing postdoctoral work at Princeton University, Szpara introduced the use of high-throughput DNA sequencing to her field, producing the first new HSV genome sequences in two decades. That provided the raw material for the first genome-wide comparative analysis of alpha-herpesviruses (the class of herpesviruses that includes HSV-1 and HSV-2), yielding valuable insights into the diversity of herpesvirus genetic sequences and protein coding ability.
Building on this work, Szpara applied the same approaches to studying a related animal herpesvirus, pseudorabies virus (PRV), and discovered several key genomic characteristics contributing to virulence and mutability in PRV. Multiple vaccine strains of PRV, including one recently sequenced by Szpara, serve as a model for HSV vaccine development.
At the same time, Szpara pursued the question of how neurons respond to pathogen infection. In mouse models of HSV-1 and PRV infection, Szpara measured genome-wide transcriptional responses (transcription being the first step in the process of gene expression, which is used by viruses to complete their lifecycles), and discovered over 2,000 significant changes in gene expression. The viral genes that cause those changes in neuronal gene expression can now be targeted with therapeutics for the development of a vaccine or cure.
At Penn State, Szpara is focused on finding causes for the range of virulence observed in human herpesvirus, which is crucial to developing a vaccine or cure with maximum efficacy. She is also looking at how HSV infection and latency affect host neurons and neighboring cells, with an eye toward finding intrinsic neuronal features and cellular defense mechanisms that may also provide targets for therapeutics to block the progression of infection.
"There are two sides to what I do," Szpara explains. "One is trying to understand the biology of herpesviruses in neurons, which has not been studied in depth. The other part of what I do is dealing with variation in this virus. What makes the strain that infects Person A different from the one that infects Person B? Why does Person A get cold sores all the time, and Person B gets them maybe once every five years? What's the difference?"
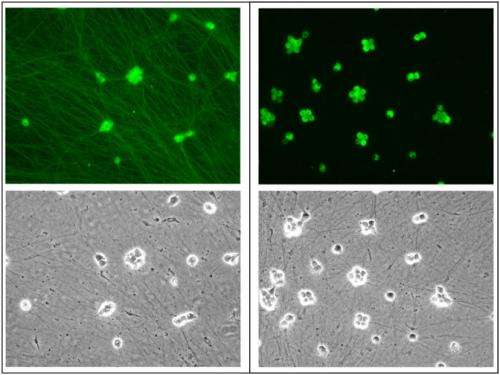
By better understanding how human herpesvirus works and what differentiates the many strains of the virus, Szpara hopes to be able to identify the specific genetic loci that contribute to virulence. And by transferring the DNA sequence fragments found at those loci between HSV strains—for example, inserting a candidate gene from a more-virulent strain into a strain that is known to be less virulent—Szpara will be able to observe the effects of that gene, in vivo in mouse models and in vitro in cultured neurons, and confirm whether it increases or reduces virulence.
"In the lab," Szpara says, "we have mouse neurons that we can culture and use as a proxy for human neurons, and we can use them to look at the cell biology of what the virus is doing and changing in those neurons. We can look at how those neurons respond and we can try to figure out if the response to a really virulent strain is different from the response to a pretty weak herpesvirus. That may be part of the puzzle of why herpesvirus outbreaks are more severe for one person than another."
Szpara's lab also uses viral genome sequencing to search for other parts of this puzzle. For this research they collect viral strains from different people, different body sites, or from cases with varying extremes of symptoms. These viruses are studied using Illumina high-throughput sequencing, and bioinformatics tools that detect the differences between strains.
"When we compare those strains to each other," says Szpara, "we try to understand exactly what in their genetic content caused them to differ in virulence. Once we've done that, we can swap the regions that differ and then test the outcome in the neurons we've cultured or into an animal model like a mouse. And if we can accurately test and prove those things, then maybe we can find a strain that's definitively weak—and weak in a way that makes it a good, safe candidate for a vaccine."

















