Study sheds light on causes of HIV dementia
A new study led by researchers at Albert Einstein College of Medicine of Yeshiva University has clarified how two major variants of HIV differ in their ability to cause neurologic complications. The finding, published in Journal of Neuroscience, highlights a new target for drugs that could prevent HIV-associated dementia, an incurable and increasingly common complication in people with AIDS. Even with anti-retroviral drug therapies, up to one-half of people infected with HIV will develop mild to moderate neurological complications, according to some estimates.
Earlier this decade, scientists observed that people with AIDS in India developed dementia at a far lower rate than comparable populations in the U.S. and Western Europe. Most cases of AIDS in India are due to infection with a subtype or clade of HIV, known as clade C, while most cases in the U.S. and Western Europe are due to clade B.
Based on these observations, in 2004, a team of researchers led by Dr. Vinayaka R. Prasad, professor of microbiology and immunology at Einstein, began searching for genetic variations between the two clades that could explain the differing rates of HIV-related dementia. The team, in collaboration with Dr. Udaykumar Ranga of the Jawaharlal Nehru Centre for Advanced Scientific Research in Bangalore, India, focused their search on Tat, a protein that helps HIV replicate and leads the attack on the brain.
Dr. Prasad and colleagues compared the sequences of the Tat protein of the two clades and noted a key difference. Where the clade B Tat protein contained the amino acid cysteine at a specific position in the Tat protein, the clade C Tat had the amino acid serine. The next step, and the focus of the current study, was to compare the two viruses in a single host to determine whether this key change in the amino acid sequence makes a practical difference in HIV's neurotoxicity.
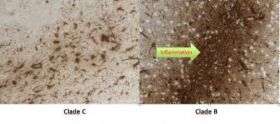
To find out, the researchers injected either clade B or clade C HIV into the brain of a special strain of immunodeficient mice. After six days--enough time for the viruses to cause neurologic damage--the mice were tested in a complex water maze that challenged their long term memory as well as their short term working memory (the type that temporarily stores and manages the information needed to carry out complex cognitive tasks, such as learning, reasoning, and comprehension).
Mice infected with clade B performed significantly worse in the maze than those infected with clade C. Moreover, when the researchers examined the mouse brains, they found more damage to neurons in the brains of mice injected with clade B than with clade C. These results were in line with the fact that people infected with clade B HIV are at greater risk for dementia than people infected with clade C.
This is the first evidence in an animal model that HIV variants from different parts of the world differ in their ability to cause neurological complications. Further, test tube studies conducted at Einstein showed strain differences in recruiting inflammatory cells to the brain. Thus, these data now provide biological evidence that Tat protein plays a crucial role in the development of HIV-related dementia.
"Tat seems to be responsible for most of the neurological symptoms seen in patients with HIV-associated dementia," says Dr. Prasad. "People have always suspected Tat to be a key protein in HIV dementia based on test tube studies. Credit for that work belongs to, among others, Dr. Joan Berman, also from Einstein. Our results, obtained using live virus in an animal model to compare genetic variants, suggest that a drug that targets HIV-1 Tat might prevent the neurological effects of AIDS."
The need for drugs that prevent HIV-dementia has grown more acute in recent years, notes Dr. Prasad. Thanks to advances in therapy, people with HIV are living increasingly longer. In 1996, a 20-year-old newly diagnosed with HIV could expect to live another 36 years, according to a recent study in The Lancet. Today, that same person could expect to live another 49 years. However, because anti-retroviral drugs do not fully eradicate HIV from the brain or the rest of the body, the low levels of virus that remain can cause significant damage.
The findings raise a larger issue, say the researchers. There appear to be significant differences between the major strains of HIV, perhaps warranting different therapeutic approaches. "Roughly 60 percent of the HIV infections worldwide are due to clade C, but all effective therapies are based on clade B," says Dr. Vasudev R. Rao, lead author of the study and research associate in microbiology and immunology at Einstein. "While our findings specifically address the differences between clade B and clade C with regard to the manifestation of HIV-associated dementia, investigating subtype differences has broad implications for clinical management and treatment for the global AIDS epidemic."
Source: Albert Einstein College of Medicine




















