Alzheimer's gene slows brain's ability to export toxic protein
The only known genetic risk factor for Alzheimer's disease slows down the brain's ability to export a toxic protein known as amyloid-beta that is central to the damage the disease causes, scientists have found.
The research, published Nov. 13 by the Journal of Clinical Investigation, provides new clues into the workings of a protein known as apolipoprotein E4, or ApoE4. People who carry two copies of the gene have roughly eight to 10 times the risk of getting Alzheimer's disease than people who do not.
The new results mark a step toward resolving a longstanding question that scientists have had about exactly how ApoE4 increases a person's risk for the disease. The findings point to differences in the way that amyloid-beta is removed from the brain depending on which ApoE protein is involved.
Scientists found that when ApoE4 is present, the brain is less efficient at ridding itself of the toxic material, because a molecule that is much slower at removing the substance becomes much more involved.
The new results are in line with a body of research amassed over the last 15 years by the leader of the team, Berislav Zlokovic, M.D., Ph.D., of the University of Rochester Medical Center, that blood circulation plays a key role in the disease. His team has identified much of the molecular machinery that allows amyloid-beta to sidestep the body's safeguards and enter the brain, and he has discovered molecules that falter when the toxic protein accumulates in the brain.
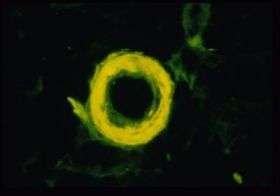
"Our latest findings help explain one of the major risk factors for Alzheimer's disease," said Zlokovic. "ApoE4 changes the brain's ability to rid itself of amyloid-beta. It's becoming more and more apparent that the brain's ability to clear out amyloid-beta, through the vascular system and across the blood-brain barrier, is central to the development of Alzheimer's disease."
In the latest work the Rochester team, working with colleagues at Washington University School of Medicine in St. Louis, found that a molecule known as very low-density lipoprotein receptor, or VLDLR, is an active – but slow – player in the removal of amyloid-beta from the brain. That step is crucial: Once amyloid-beta gets out of the brain and into the body, it can be eliminated easily.
"It's as if you have a pile of trash building up in the brain, and you need to move the trash away before it becomes toxic," said Rashid Deane, Ph.D., one of the authors of the paper and research professor of Neurosurgery at the University of Rochester Medical Center.
"We've known that the brain uses a molecule called LRP1, which is extremely efficient and acts like a fast ferry to remove amyloid-beta. Now we've found that there is another molecule involved, which works much more slowly, and it's especially active when amyloid is coupled to ApoE4," Deane added.
The team showed that speedy LRP1 is central to removing amyloid-beta when ApoE2 or ApoE3 is involved, with the slower VLDLR picking up some of the slack. But when the form of the gene that puts people at risk, ApoE4, is involved, VLDLR nearly alone is responsible for hauling the amyloid-beta away.
"It's like having a choice between a fast ferry and a slow ferry," said Deane. "For reasons we don't yet understand, when ApoE4 is involved, the slow ferry is used almost exclusively. This means that the amyloid-beta isn't removed as quickly as it otherwise would, potentially giving it a chance to accumulate, like we see in the brains of patients with Alzheimer's disease."
The team found that LRP1 is able to export amyloid from the brain about 20 times faster than VLDLR. Consequently, in mice with the more efficient versions of the ApoE protein, ApoE2 and ApoE3, amyloid is cleared out of the brain at a rate about twice or three times as fast as it is in mice with the ApoE4 protein. Amyloid deposits accumulate in the brains of mice with the ApoE4 protein in much higher amounts, about 10 to 15 times as much as in the brains of mice with either ApoE2 or ApoE3.
Not only do the ApoE proteins help determine how quickly amyloid-beta is removed from the brain; the proteins actually couple with amyloid-beta in the brain to form sticky complexes. This gunk gathers around cells and is much more difficult to remove from the brain than free-floating amyloid-beta. Companies are trying to develop drugs that would break up the relationship, freeing amyloid-beta and making it easier to remove from the brain.
Source: University of Rochester Medical Center





















