A strange case of upper obstructive syndrome
Aorto-duodenal fistulae (ADF) are the most frequent aorto-enteric fistulae (80%) and the most frequent presenting sign of ADF is upper gastrointestinal bleeding (UGI). A 59-year-old male patient, who underwent an aortic-bi-femoral bypass five years ago, was admitted to the Emergency Room after five days of persistent occlusive syndrome with dyspepsia and biliary vomiting.
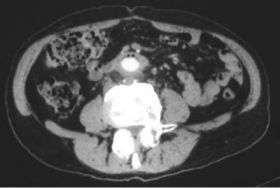
Computed tomography (CT) scan showed in the third duodenal segment the presence of an area with the characteristics of inflammatory tissue, including air bubbles between the duodenum and aortic-bi-femoral prosthesis adherent to the third duodenal portion (¡°comma sign¡±). Microbiological cultures and scintigraphy were unremarkable. Esophago-gastro-duodenoscopy showed the aortic prosthesis crossing the third segment of duodenal wall occluding the intestinal lumen. At laparotomy, after viscerolisis, the prosthesis was detached from duodenal wall and the intestine failed to close transversely.
To protect the intestinal wall, a pediculated fragment of the greater omentum was placed between the duodenum and aortic bypass. Furthermore, a gastrojejunal Roux anastomosis was employed. The prosthesis was not changed because there were no local or systemic signs of infection. The post-operative course was uneventful.
These findings were published in the January 21, 2008 edition of the World Journal of Gastroenterology. ADF may be primarily due to a spontaneous communication between the lumen of aortic aneurysm and intestinal loop, or secondarily due to surgical repair of aneurysms with prosthetic implants. Clinical suspicion is essential in the diagnosis of ADF and the most commonly used techniques for its diagnosis are esophago-gastro-duodenoscopy (EGDS) and CT.
Otherwise, secondary ADF is an uncommon (0.3% - 2%) and life-threatening long-term complication of aortic reconstructive surgery, with only hypothetic and speculative pathogenesis (mechanical erosion, lack of interposed retroperitoneal tissue, excessive pulsation of redundantly placed grafts, septic procedures by Staphylococcus epidermidis ¡°biofilm¡± infection, inadequate prosthetic materials).
In our case, ADF formation was related to graft pulsation on the duodenal wall.
The presentation is often subtle, with herald bleeding followed by a period of grace, or catastrophic bleeding, or rarely an episode of intestinal obstruction. The third or fourth duodenal segment is the most frequently involved site. In Dacron prosthesis patients, fistula develops in the proximal graft tract opening in the third segment of duodenum.
Because of the high mortality and morbidity associated with secondary aorto-enteric fistula, surgical treatment is always recommended. Explorative laparotomy is the treatment of choice. In the case of non-treated aortic-enteric fistula presenting with massive UGI-bleeding, the mortality rate is near 100%. Morbidity (limb loss in 10% - 40%) and mortality related to treated ADF are also high (75%) and require preventive measures, including more particularly delicate surgery and antibiotic therapy in case of infection. Several surgical procedures are possible.
Source: World Journal of Gastroenterology




















