Bone marrow cells that transform into skin cells could revolutionise approach to wound treatment
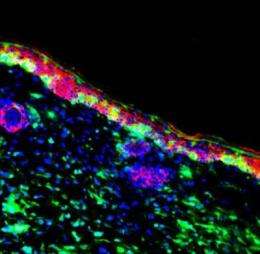
Researchers at King's College London and Osaka University in Japan have identified specific bone marrow cells that can transform into skin cells to repair damaged skin tissue, according to a study published in Proceedings of the National Academy of Sciences (PNAS).
The team has uncovered how this process works, providing new insights into the mechanisms behind skin repair. This significant advance has the potential to revolutionise approaches to wound treatment in the future, which could benefit people with chronic wounds such as leg ulcers, pressure sores and burns, as well as genetic skin diseases such as epidermolysis bullosa, which causes painful blisters on the skin.
The current management of chronic wounds in UK patients costs more than a billion pounds every year so this new scientific discovery could lead to significant future cost savings for the NHS.
It was already known that bone marrow may play a role in skin wound healing, but until now it was not known which specific bone marrow cells this involves, how the process is triggered, and how the key cells are recruited to the affected skin area. The team of researchers carried out experiments in mice, specifically looking at the mechanisms involved when skin grafts are used, compared with non-grafted wound healing.
The findings showed that in mice with non-grafted wound healing, very few bone marrow cells travelled to the wound to repair it and they did not make a major contribution to epidermal repair. But in mice where a skin graft was used, a significantly higher number of specific bone marrow-derived cells travelled to the skin graft to heal the area more quickly and build new skin directly from the bone marrow cells.
The research showed that around one in every 450 bone marrow cells has the capacity to transform into skin cells and regenerate the skin.
The team also identified the signal that triggers recruitment of the bone marrow cells to repair skin. Damaged skin can release a distress protein called HMGB1 that can mobilise the cells from bone marrow and direct them to where they are needed.
Mice with skin grafts express high levels of HMGB1 in their blood that can drive the bone marrow repair process. The findings provide new insight into how skin grafts work in medicine – they do not simply cover wounds, but act as bioreactors that can kick-start regenerative skin repair.
The research also showed that patients with epidermolysis bullosa have high levels of HMGB1 in their blood and that the source here is the roofs of the blisters in their skin. This finding demonstrates that HMGB1 is also important in human skin damage and wound healing responses.
Professor John McGrath, Head of the Genetic Skin Disease Group at King's, recently spent several months working on the project in Osaka. He said: "This work is tremendously exciting for the field of regenerative medicine. The key achievement has been to find out which bone marrow cells can transform into skin cells and repair and maintain the skin as healthy tissue, and to learn how this process happens.
"Understanding how the protein HMGB1 works as a distress signal to summon these particular bone marrow cells is expected to have significant implications for clinical medicine, and could potentially revolutionise the management of wound healing.
"Chronic wounds and tissue injury represent a significant cost to the NHS, not to mention the debilitating effects on peoples' quality of life. Our plan is to see if we can now use this scientific advance to develop more effective treatments to improve tissue repair in skin and perhaps other organs."
Professor McGrath is working together with colleagues at Osaka University to harness the key parts of the HMGB1 protein to create a drug treatment that can augment tissue repair. It is expected that the developed treatment will be tested in animal models in about a year and enter clinical trials shortly afterwards.















