On the trail of a stealthy parasite
About one-third of the human population is infected with a parasite called Toxoplasma gondii, but most of them don’t know it.
Though Toxoplasma causes no symptoms in most people, it can be harmful to individuals with suppressed immune systems, and to fetuses whose mothers become infected during pregnancy. Particularly dangerous strains, found mainly in South America, are the leading cause of blindness in Brazil.
Toxoplasma is one of the very few parasites that can infect nearly any warm-blooded animal. Its spores are found in dirt and easily infect farm animals such as cows, sheep, pigs and chickens. Humans can be infected by eating undercooked meat or unwashed vegetables.
“It’s everywhere, and you just need one spore to become infected,” says Jeroen Saeij, an assistant professor of biology at MIT. “Most cases don’t kill the host but establish a lifelong, chronic infection, mainly in the brain and muscle tissue.”
Saeij is investigating a key question: why certain strains of the Toxoplasma parasite (there are at least a dozen) are more dangerous to humans than others.
He and his colleagues have focused their attention on the type II strain, which is the most common in the United States and Europe, and is also the most likely to produce symptoms. In a paper appearing in the Jan. 3 online edition of The Journal of Experimental Medicine, the researchers report the discovery of a new Toxoplasma protein that may help explain why type II is more virulent than others.
A stealthy infection
Toxoplasma infection rates vary around the world. In the United States, it’s about 10 to 15 percent, while rates in Europe and Brazil are much higher, around 50 to 80 percent. However, these are only estimates — it is difficult to calculate precise rates because most infected people don’t have any symptoms.
After an infection is established, the parasite forms cysts, which contain many slowly reproducing parasites, in muscle tissue and the brain. If the cysts rupture, immune cells called T cells will usually kill the parasites before they spread further. However, people with suppressed immune systems, such as AIDS patients or people undergoing chemotherapy, can’t mount an effective defense.
“In AIDS patients, T cells are essentially gone, so once a cyst ruptures, it can infect more brain cells, which eventually causes real damage to the brain,” says Saeij.
The infection can also cause birth defects, if the mother is infected for the first time while pregnant. (If she is already infected before becoming pregnant, there is usually no danger to the fetus.)
There are drugs that can kill the parasite when it first infects someone, but once cysts are formed, it is very difficult to eradicate them.
Path to inflammation
A few years ago, Saeij and colleagues showed that the Toxoplasma parasite secretes two proteins called rhoptry18 and rhoptry16 into the host cell. Those proteins allow the parasite to take over many host-cell functions.
“That was a major earthquake in the field,” says Eric Denkers, professor of immunology at Cornell University College of Veterinary Medicine, who was not involved in the new MIT paper. “This paper will be a major aftershock.”
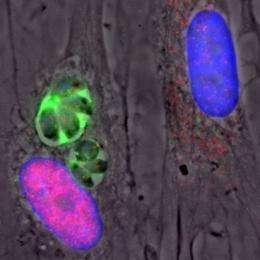
In the new study, the MIT team showed that the parasite also secretes a protein called GRA15, which triggers inflammation in the host. All Toxoplasma strains have this protein, but only the version found in type II causes inflammation, an immune reaction that is meant to destroy invaders but can also damage the host’s own tissues if unchecked. In the brain, inflammation can lead to encephalitis. This ability to cause inflammation likely explains why the type II strain is so much more hazardous for humans, says Saeij.
Saeij and his team, which included MIT Department of Biology graduate students Emily Rosowski and Diana Lu, showed that type II GRA15 leads to the activation of the transcription factor known as NF-kB, which eventually stimulates production of proteins that cause inflammation. The team is now trying to figure out how that interaction between GRA15 and NF-kB occurs, and why it is advantageous to the parasite.
Ultimately, Saeij hopes to figure out how the parasite is able to evade the immune system and establish a chronic infection. Such work could eventually lead to new drugs that block the parasite from establishing such an infection, or a vaccine that consists of a de-activated form of the parasite.
For press release but not for story: MIT Department of Biology graduate students Emily Rosowski and Diana Lu are the paper’s two first authors and contributed equally to the research. Other authors include MIT postdoc Kirk Jensen, lab technician Lindsay Julien, MIT undergraduate student Lauren Rodda, and Rogier Gaiser, a graduate student at Wageningen University in the Netherlands.
This story is republished courtesy of MIT News (web.mit.edu/newsoffice/), a popular site that covers news about MIT research, innovation and teaching.
More information: "Strain-specific activation of the NF-kB pathway by GRA15, a novel Toxoplasma gondii dense granule protein," by Emily E. Rosowski, Diana Lu, Lindsay Julien, Lauren Rodda, Rogier A. Gaiser, Kirk D.C. Jensen, Jeroen P.J. Saeij. Journal of Experimental Medicine, 3 January 2011.

















