Detecting esophageal cancer with light
A tiny light source and sensors at the end of an endoscope may provide a more accurate way to identify pre-cancerous cells in the lining of the esophagus.
Developed by biomedical engineers at Duke University and successfully tested on patients during a clinical trial at the University of North Carolina at Chapel Hill, the device holds the promise of being a less invasive method for testing patients suspected of having Barrett's esophagus, a change in the lining of the esophagus due to acid reflux. Acid reflux occurs when stomach acid splashes, or refluxes, up into the esophagus.
Long periods of acid reflux can change the cells that line the esophagus, making them appear more like intestinal cells than esophageal cells. These cellular changes can also be a precursor to cancer. As in most cancers, early identification of these pre-cancerous cells often leads to better outcomes for patients. Barrett's esophagus afflicts more than one percent of the U.S. population, with most patients above the age of 50.
Using an endoscope to reach the esophagus via the nose, physicians shine short bursts of this light at locations of suspected disease and sensors capture and analyze the light as it is reflected back. In particular, they are trying to spot characteristic changes within the layer of cells known as the epithelium, which line cavities and surfaces throughout the body.
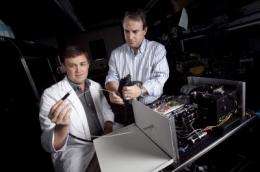
"By interpreting the way the light scatters after we shine it at a location on the tissue surface, we can the spot the tell-tales signs of cells that are changing from their healthy, normal state to those that may become cancerous," said Neil Terry, a Ph.D. student working in the laboratory of Adam Wax, associate professor of biomedical engineering at Duke's Pratt School of Engineering, who developed the device.
The team published their findings online in the January issue of the journal Gastroenterology.
"Specifically, the nuclei of pre-cancerous cells are larger than typical cell nuclei, and the light scatters back from them in a characteristic manner," Terry continued. "When we compared the findings from our system with an actual review by pathologists, we found they correlated in 86 percent of the samples."
UNC gastroenterologist Nicholas Shaheen, M.D., conducted the preliminary clinical trial of the device on 46 patients with Barrett's esophagus.
"Currently, we take many random tissue samples from areas we where we think abnormal cells may be located," Shaheen said. "This new system may make our biopsies smarter and more targeted. Early detection is crucial, because the cure rate for esophageal cancer that is caught early is quite high, while the cure rate for advanced disease is dismal, with a 15 percent survival rate after five years."
The technology that Wax and his team developed for cancer detection is known as angle-resolved low coherence interferometry (a/LCI). The technique is able to separate the unique patterns of the nucleus from the other parts of the cell and provide representations of its changes in shape in real time.
"This optical approach of sampling allows us to cover more tissue sites in less time and has the potential to significantly improve our ability to spot and monitor these pre-cancerous cells," Wax said. "This type of approach could be used to improve and perhaps one day supplant the physical biopsies currently being used."
Wax pointed out that since approximately 85 percent of all cancers begin within the layers of the epithelium in various parts of the body, he believes that the new system could also work in such cancers as those of the colon, trachea, cervix or bladder.














