UCLA team uncovers mechanism behind organ transplant rejection
UCLA researchers have pinpointed the culprit behind chronic rejection of heart, lung and kidney transplants. Published in the Nov. 23 edition of Science Signaling, their findings suggest new therapeutic approaches for preventing transplant rejection and sabotaging cancer growth.
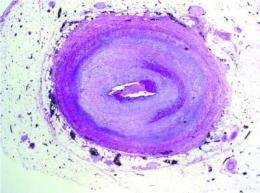
The team focused on the mechanism behind narrowing of the donor's grafted blood vessels, which blocks blood from reaching the transplanted organ. Starved of oxygen and other nutrients, the organ eventually fails, forcing the patient back on the transplant waiting list.
"Chronic rejection is the No. 1 cause of organ failure in the first year of transplant," explained Elaine Reed, director of the UCLA Immunogenetics Center and professor of pathology at the David Geffen School of Medicine at UCLA. "In the first five years, some 40 percent of organs fail after transplant due to blockage of the grafted blood vessels. Currently, we have no way to treat this deadly condition."
Earlier research by Reed's laboratory discovered that patients whose immune systems manufactured antibodies to their donor's human leukocyte antigens (HLA) were at higher risk for chronic rejection.
In this study, Reed and her colleagues looked at how HLA molecules on donor tissue provoke an immune response in the patient. The team examined how the patient's antibodies trigger signals that spark overgrowth of the cells lining the inner blood vessels of the grafted organ.
The scientists discovered that HLA's ability to stimulate cell growth and movement depends upon a quid pro quo relationship with another molecule called integrin beta 4.
"Integrin enables cells to survive and spread, which is essential for tumor progression," said Reed. "We suspect that integrin hijacks HLA and takes over its functions. When we suppressed integrin, HLA was unable to make cells grow and move."
Conversely, when the team suppressed HLA, integrin could no longer support cells' communication with their environment. The finding implies that HLA is required for functions regulated by integrin, such as cellular movement.
"Ours is the first study to demonstrate a physical and functional liaison between HLA and integrin," said Reed. "HLA's role in helping integrin is a completely new function that has never been described before."
The UCLA findings offer valuable insight into the molecular mechanisms that allow HLA to stimulate cellular growth and movement.
"What I'm excited about from a medical point of view is how our findings offer new therapeutic opportunities," said Reed. "If we can identify ways to disrupt the relationship between HLA and integrin, we may be able to prevent chronic organ rejection in transplant patients."
The UCLA team's next step will be to investigate how integrin and HLA function together to promote cancer growth. The research suggests a new approach for halting cancer progression by preventing angiogenesis, the process by which a tumor develops its own blood supply.
"By interfering with integrin's reliance upon HLA to signal cells, we can sabotage cells' ability to sprout new blood vessels to feed the tumor," observed Reed.
















