Antibiotics take toll on beneficial microbes in gut
It's common knowledge that a protective navy of bacteria normally floats in our intestinal tracts. Antibiotics at least temporarily disturb the normal balance. But it's unclear which antibiotics are the most disruptive, and if the full array of "good bacteria" return promptly or remain altered for some time.
In studies in mice, University of Michigan scientists have shown for the first time that two different types of antibiotics can cause moderate to wide-ranging changes in the ranks of these helpful guardians in the gut. In the case of one of the antibiotics, the armada of "good bacteria" did not recover its former diversity even many weeks after a course of antibiotics was over.
The findings could eventually lead to better choices of antibiotics to minimize side effects of diarrhea, especially in vulnerable patients. They could also aid in understanding and treating inflammatory bowel disease, which affects an estimated 500,000 to 1 million Americans, and Clostridium difficile, a growing and serious infection problem for hospitals.
Normally, a set of thousands of different kinds of microbes lives in the gut - a distinctive mix for each person, and thought to be passed on from mother to baby. The microbes, including many different bacteria, aid digestion and nutrition, appear to help maintain a healthy immune system, and keep order when harmful microbes invade.
"Biodiversity is a well-known concept in the health of the world's continents and oceans. Diversity is probably important in the gut microsystem as well," says Vincent B. Young, M.D., Ph.D., senior author of the study, which appears in the June issue of Infection and Immunity.
The study results suggest that unless medical research discovers how to protect or revitalize the gut microbial community, "we may be doing long-term damage to our close friends," says Young, assistant professor in the departments of internal medicine and microbiology and immunology at the U-M Medical School.
Study details
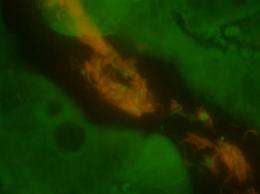
Young and his colleagues used a culture-independent technique, using sequence analysis of 16S rRNA-encoding gene libraries, to profile the bacterial communities in the gut. It allows them to look for many more kinds of microbes than was possible with more limited methods. The result is a much more complete picture of the diversity of microbes in the gut.
Mice, which normally develop a diverse set of microbes after being born without one, then were given either cefoperazone, a broad-spectrum cephalosporin antibiotic, or a combination of three antibiotics (amoxicillin, bismuth and metronidazole). The scientists then observed what changes in the gut microbiota occurred immediately after the antibiotics were stopped or six weeks following the end of treatment.
"Both antibiotic treatments caused significant changes in the gut microbial community. However, in the mice given cefoperazone, there was no recovery of normal diversity. In other mice given the amoxicillin-containing combination, the microbiota largely recovered, but not completely," says Young.
However, Young's team found that a little socializing sparked recovery in even the most severely affected mice. Some of the mice given cefoperazone soon recovered normal microbes after an untreated mouse was placed in the same cage. That wasn't a complete surprise, since mice have a habit of eating the feces of their cage mates and therefore picked up normal gut microbes quickly.
Not a lesson applicable to humans? In patients with refractory antibiotic-associated diarrhea due to C. difficile, there have been limited trials of treatments using "fecal transplants" to replace lost gut microbiota. Although this is a pretty unpalatable treatment at first glance, the clinical response was quite remarkable, Young says.
Implications
Although cefaperazone is not commonly used in the United States, related drugs such as cefoxitin are. The study findings suggest that it is really important to use antibiotics only when indicated, especially in people with health problems that might already compromise their gut microbe health, Young says. Multiple rounds of antibiotics may also deserve concern.
The findings will guide Young in related work in which he is using mouse models to examine how changes in the microbiota in the gut may influence how inflammatory bowel disease develops and progresses. The study will also inform ongoing research in his lab to gain insights into colitis associated with C. difficile infection. The Young laboratory recently published a study that demonstrates that long-term decreases in gut microbe diversity from repeated antibiotics are associated with recurring C. difficile infection in human patients.
Young cautions against concluding that popular probiotics supplements necessarily are safe and effective for everyone looking for a way to restore healthy gut microbes. An individual's specific health needs and vulnerabilities have to be considered. "Probiotics may be part of the solution, but we don't know that yet," he says.
Source: University of Michigan Health System (news : web)














